In a groundbreaking study published in Nature Communications, researchers have paved the way toward a deeper understanding of the complex interplay between lipid metabolism and neuroinflammatory responses in the brain. The study specifically dissects the consequences of sulfatide deficiency in the central nervous system and its association with astrogliosis and myelin lipid dysregulation. Contrary to previous assumptions, the findings reveal these pathological changes occur independently of TREM2-mediated microglial activation—a discovery that challenges current paradigms on neuroimmune interactions and may redefine therapeutic strategies for demyelinating diseases.
Sulfatides, a class of sulfated galactosylceramides, are indispensable lipid components of myelin sheaths, contributing fundamentally to their stability and function. Their deficiency has long been implicated in neurodegenerative disorders, especially those characterized by white matter abnormalities. What remained unclear was the precise cellular mechanisms leading to glial activation and myelin lipid imbalance as a consequence of sulfatide depletion. This study, through a robust combination of lipidomic profiling, genetic models, and mechanistic exploration, sheds light on these critical aspects.
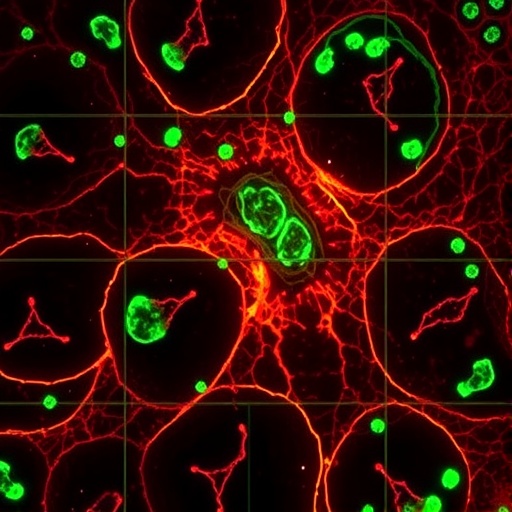
The researchers utilized genetically engineered mouse models exhibiting targeted sulfatide deficiency, providing an in vivo system to mimic pathological conditions associated with disrupted myelin integrity. Comprehensive lipidomic analyses revealed profound perturbations in myelin-associated lipid species, extending beyond sulfatide depletion to involve broader lipid homeostasis disturbances. These alterations in lipid content and composition manifest as compromised myelin sheath integrity and altered membrane dynamics, setting the stage for downstream cellular responses.
Astrogliosis, characterized by hypertrophy and proliferation of astrocytes, emerged as a pronounced response to sulfatide insufficiency. This robust activation of astrocytes potentially reflects a compensatory or pathological reaction to the destabilized lipid environment within the myelin. Intriguingly, despite the well-established role of microglia in neuroinflammatory processes and myelin clearance, the anticipated activation of microglia through the TREM2 receptor was surprisingly absent. TREM2, a receptor critical for microglial sensing and signaling in various neurodegenerative contexts, appeared dispensable under these conditions.
Further detailed investigations confirmed that microglial populations failed to exhibit hallmark activation signatures commonly mediated by TREM2 signaling pathways. This dissociation between sulfatide deficiency-induced astrogliosis and TREM2-dependent microgliosis indicates the existence of alternative mechanistic pathways driving astrocyte reactivity independently from microglial influence. This discovery opens new avenues for exploring astrocyte-intrinsic lipid-sensing mechanisms that might trigger astrogliosis.
Moreover, the study identifies a distinct molecular milieu within astrocytes, possibly orchestrated by altered lipid metabolites or membrane perturbations, which drive these cells toward a reactive phenotype. These findings suggest that astrocytes possess intrinsic lipid-sensitive pathways capable of responding directly to myelin lipid imbalance—a perspective that elevates their role from passive support cells to active participants in neurodegenerative pathologies.
The dissociation of myelin lipid dysregulation and astrogliosis from TREM2-dependent microglial activation has profound implications for therapeutic development. Drugs targeting microglial TREM2 activity are being designed for conditions like Alzheimer’s disease and multiple sclerosis, based on assumptions that microglia are principal mediators of lipid-driven neuroinflammation. This study cautions against this oversimplification, emphasizing that such approaches may inadequately address astrocyte-mediated pathological processes.
From a methodological standpoint, the study employed cutting-edge lipidomic techniques, including mass spectrometry imaging and shotgun lipidomics, to capture a high-resolution landscape of lipid perturbations. Coupling these methods with transcriptomic analyses allowed researchers to correlate lipid anomalies with gene expression changes within glial populations, unveiling intricate molecular signatures underlying the observed phenotypes.
Additionally, experiments employing TREM2 knockout models and specific pharmacological inhibitors ensured the rigor of conclusions regarding microglial independence. This methodological rigor underscores the robustness of the findings and sets a foundation for future studies to explore alternative glial signaling and activation mechanisms beyond canonical microglial receptors.
The implications of this research extend into clinical contexts, particularly for demyelinating disorders such as multiple sclerosis and leukodystrophies. Understanding how sulfatide deficiency precipitates astrocytic changes without involving microglial pathways suggests that therapeutic targeting of astrocyte-specific responses and lipid metabolism may be a more promising strategy than microglial modulation in certain stages or forms of these diseases.
Furthermore, this work fuels the growing recognition of lipid metabolism as a critical driver of central nervous system health and disease. The dynamic regulation of myelin lipids and their metabolites emerges as a nexus of cellular communication and pathology, reshaping views on how glial cells detect and respond to homeostatic disturbances.
In summary, this landmark study challenges existing dogma regarding microglial involvement in sulfatide deficiency-induced neuroinflammation, instead highlighting the pivotal role of astrocytes as mediators of pathological astrogliosis and lipid dyshomeostasis. The independence from TREM2 signaling not only redefines the mechanistic landscape but also calls for broader consideration of glial heterogeneity and lipid-centric interventions in neurodegenerative diseases.
As research in neuroimmunology advances, studies like this underscore the necessity of dissecting cell-type specific contributions to disease, particularly in the sophisticated and lipid-rich environment of the central nervous system. By unraveling the distinct pathways linking lipid metabolism and glial activation, we edge closer to designing precision therapies that halt or reverse the progression of debilitating neurological conditions.
This novel insight into sulfatide deficiency-induced pathology represents a pivotal leap forward, painting a more nuanced picture of glial biology and myelin integrity. With an enhanced understanding of astrocyte-driven disease processes, future explorations may unlock new biomarkers and intervention points with the potential to transform patient outcomes in diseases traditionally dominated by microglial-centric narratives.
Subject of Research: The study investigates the impact of sulfatide deficiency on astrocyte activation (astrogliosis) and myelin lipid homeostasis, particularly exploring whether these changes are dependent on TREM2-mediated microglial activation processes.
Article Title: Sulfatide deficiency-induced astrogliosis and myelin lipid dyshomeostasis are independent of TREM2-mediated microglial activation.
Article References:
He, S., Mittra, N., Bao, H. et al. Sulfatide deficiency-induced astrogliosis and myelin lipid dyshomeostasis are independent of TREM2-mediated microglial activation. Nat Commun 17, 338 (2026). https://doi.org/10.1038/s41467-025-66222-9
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41467-025-66222-9
Tags: astrogliosis and lipid metabolismbrain lipid metabolism and myelin stabilitygenetically engineered mouse models in neuroscienceglial activation mechanisms in CNSlipidomic profiling in brain researchmyelin lipid dysregulationneurodegenerative disorders and white matter abnormalitiesneuroimmune interactions in glial cellssulfatide deficiency and neuroinflammationsulfatides and central nervous system healththerapeutic strategies for demyelinating diseasesTREM2-independent microglial activation