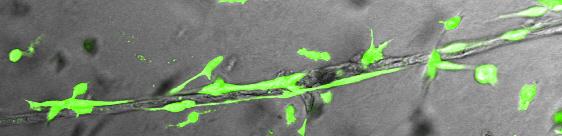
Credit: Image courtesy of Akhilesh Kumar, Wisconsin National Primate Research Center
MADISON, Wisconsin — In the average adult human, there are an estimated 100,000 miles of capillaries, veins and arteries — the plumbing that carries life-sustaining blood to every part of the body, including vital organs such as the heart and the brain.
When things go wrong with vasculature, the result can be a heart attack, stroke or other life-threatening or chronic condition. An estimated 8.5 million people in the United States alone have diseased arteries, and diseases of the blood vessels kill more people worldwide than any other condition.
But now scientists are poised to get a better look at the fundamental development of the cells that make up blood vessels and how they can be more reliably cultured in the laboratory dish. Writing this week (May 30, 2017) in Cell Reports, a team led by Igor Slukvin, a University of Wisconsin-Madison professor of pathology and laboratory medicine, and cell and regenerative biology, describes the developmental pathway that gives rise to the different types of cells that make up human vasculature.
"If you know how cells develop, you can design appropriate therapies," Slukvin explains. "We have been able to develop the conditions to make these different types of cells in the lab."
The advance reported by Slukvin's team, with lead author Akhilesh Kumar, a staff scientist with the Wisconsin National Primate Research Center, is important because it provides a blueprint for how vasculature arises at the earliest stages of development. Now, scientists can study the cells that compose blood vessels and devise new models for studying blood vessel disease. Critically, the discovery of methods to generate the building block-cells could help set the stage for engineering blood vessels in the laboratory for disesase modeling, drug screening and therapeutic purposes.
Access to the cells that compose blood vessels and knowing their developmental pathway as they arise from a common progenitor — known as a mesenchymoangioblast — to become endothelial and mesenchymal cells, helps solve a fundamental problem in blood vessel tissue engineering: providing ready access to sources of cells to grow vessels for therapy.
"Now, investigators will have access to a plethora of new cell type alternatives for vascular engineering," says Kumar, noting that the new Wisconsin study, paired with the native abilities of the progenitor stem cells to proliferate and differentiate to different cell types in culture, can potentially accelerate the time it takes to grow vascular grafts.
A central finding in the new study is the discovery of cell markers to identify the different types of cells in the lab dish. Scientists can identify the different types of vascular cells in living tissue. For example, pericytes are associated with small vessels such as capillaries, while smooth muscle cells contribute to the vascular wall of larger vessels. However, when cells are made de novo in culture, it was difficult to distinguish one cell type from another.
"In the body, we can identify the cells by location," notes Slukvin, whose faculty appointment is in the UW School of Medicine and Public Health. "We couldn't do that in the lab dish. We needed to identify the cell-type specific markers."
In the study, Kumar found that cells that compose blood vessels arise from the common mesenchymoangioblast progenitor, a cell type that also gives rise to tissues such as bone, cartilage and muscle. The ability to trace the developmental pathway that gives rise to the cells that make up blood vessels gives science a potent pathway to devise new cellular therapies: "If you know how cells develop, we can design appropriate therapies," Slukvin says.
Now, blood vessels and arteries used to treat patients often come from the patients themselves. Creating new blood vessels from scratch for therapy is still far from reality, but the new Wisconsin study is an essential step toward that goal. Engineering tissue for therapy is a drawn-out process, but the use of induced pluripotent stem cells to create tissue banks from patients whose genetic profiles make them compatible donors for most people is a strategy being actively explored, including by a Morgridge Institute for Research collaboration led by Wisconsin stem cell pioneer Jamie Thomson, a co-author of the new study.
More immediate application of the research, says Slukvin, lies in being able to create laboratory models for vascular disease. The models will inform a better basic understanding of what goes wrong in killers such as coronary artery disease and genetic diseases that affect vasculature. Moreover, the cells can be used in high-throughput drug screens, accelerating the pace of development of new drugs and repurposing old ones to treat vascular ailments.
###
Terry Devitt, (608) 262-8282, [email protected]
This work was supported by funds from the National Institutes of Health (U01HL099773, P01 GM081629 and P51 OD011106) and the Charlotte GeyerFoundation. Disclosure: Slukvin is a founding shareholder and consultant for Cynata, an Australian stem cell and regenerative medicine company.
Media Contact
Igor Slukvin,
[email protected]
608-263-0058
@UWMadScience
http://www.wisc.edu
############
Story Source: Materials provided by Scienmag