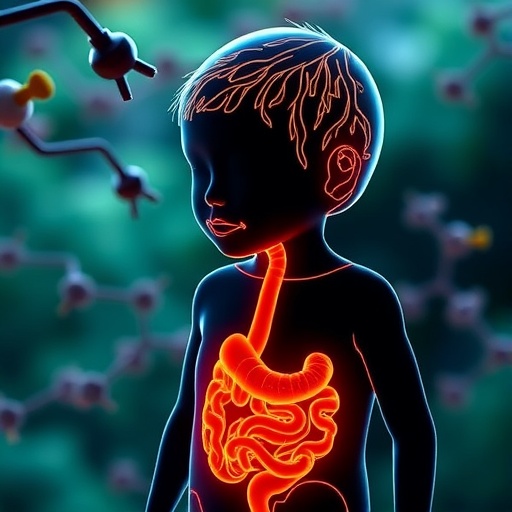
In a groundbreaking stride towards personalized healthcare, the latest research in pediatric inflammatory bowel disease (IBD) unveils the transformative potential of small-molecule therapies. This innovative approach, detailed in the recent publication by Chen et al. in the World Journal of Pediatrics, marks a significant shift from conventional treatment paradigms. As pediatric IBD continues to pose complex challenges due to its chronic and multifactorial nature, the promise of precision medicine driven by small molecules offers a beacon of hope for tailored, effective care.
Inflammatory bowel disease, encompassing Crohn’s disease and ulcerative colitis, disproportionately affects children and adolescents with symptoms that severely impair quality of life. Traditionally managed with broad immunosuppressive agents, pediatric IBD treatments often grapple with issues of variable efficacy and significant side effects. The advent of small-molecule therapeutics is revolutionizing this landscape by targeting specific molecular pathways implicated in the disease, potentially enhancing therapeutic precision and minimizing adverse outcomes.
Small molecules, defined by their low molecular weight and ability to penetrate cells easily, stand out for their versatility and oral bioavailability. Unlike biologics, which are typically large protein molecules requiring injections, small-molecule drugs can modulate intracellular targets, offering a strategic advantage in interfering with cellular mechanisms that underlie inflammation and immune dysregulation in IBD. This characteristic pivotal to their rapid absorption and distribution heralds a new era of accessible and patient-friendly treatment options.
Central to this therapeutic evolution is the identification of molecular targets critical to the pathogenesis of pediatric IBD. The inflammatory cascade in IBD involves various signaling molecules such as cytokines, kinases, and transcription factors. Small molecules are ingeniously designed to inhibit or modulate these targets, damping inappropriate immune responses while preserving systemic immunity. Such specificity is crucial in children who are still developing and vulnerable to systemic immunosuppression-related complications.
A fascinating facet of this research is the integration of genetic and molecular profiling to stratify pediatric patients. By harnessing precision medicine techniques, clinicians can identify specific biomarkers or gene signatures that predict responsiveness to certain small molecules. This stratification not only optimizes therapeutic outcomes but also reduces unnecessary exposure to ineffective treatments, thus aligning clinical decisions with individual patient biology.
Emerging small-molecule agents include Janus kinase (JAK) inhibitors, sphingosine-1-phosphate receptor modulators, and phosphodiesterase inhibitors, each exerting effects through distinct pathways. JAK inhibitors, for example, interfere with intracellular signaling crucial for the function of various pro-inflammatory cytokines integral to IBD pathology. Their ability to attenuate inflammation without broadly suppressing immune function represents a substantial advancement in managing pediatric IBD’s complexities.
The clinical development pipeline showcases promising data from trials involving these agents, with preliminary results highlighting improved remission rates and reduced disease activity scores in children. Importantly, their safety profiles appear favorable compared to traditional immunomodulators, a vital consideration given the long-term treatment horizons in pediatric populations. Such evidence supports regulatory momentum toward approving these drugs for clinical use in younger patients.
Moreover, the article emphasizes the importance of understanding the pharmacokinetics and pharmacodynamics of small molecules in children, whose metabolic pathways differ significantly from adults. Tailoring dosing regimens to pediatric physiology is imperative to maximize efficacy while minimizing toxicity. The research community is actively addressing these challenges through advanced modeling and sophisticated clinical trial designs explicitly focusing on pediatric cohorts.
Another critical insight from this work is the role of the gut microbiome in modulating drug response. Small molecules can influence not only immune cells directly but also the microbial environment within the gastrointestinal tract, which in turn affects inflammation and disease progression. This bidirectional interplay underscores the necessity of integrated therapeutic strategies that consider both host and microbial factors for achieving durable remission.
The precision medicine approach in pediatric IBD heralds an era where treatment is no longer a one-size-fits-all model but a customized regimen sculpted to each child’s molecular profile. This aligns with broader trends in medicine aiming to harness genomic, proteomic, and metabolomic data for highly specific interventions. Such a paradigm shift promises to transform clinical outcomes and quality of life for children grappling with this debilitating disease.
Despite these remarkable advancements, challenges remain. The heterogeneity of pediatric IBD, both genetically and phenotypically, demands continuous discovery of novel molecular targets and the development of next-generation small molecules. Additionally, long-term studies are essential to ascertain the safety and effectiveness of these therapies over the course of childhood and adolescence, ensuring that the benefits outweigh potential risks.
Future research directions will likely focus on combinatorial therapies, whereby small molecules are paired with biologics or other modalities to achieve synergistic effects. This multifaceted approach may overcome resistance mechanisms and fine-tune immune modulation. Moreover, leveraging artificial intelligence and machine learning to analyze large datasets could accelerate biomarker discovery and personalized treatment algorithms.
In conclusion, the advent of small-molecule therapies marks a significant milestone in the quest for precision medicine in pediatric inflammatory bowel disease. By intricately targeting the molecular underpinnings of IBD, these agents offer new hope for children worldwide, promising not only improved symptom control but also a path toward sustained remission with fewer side effects. As the scientific community continues to unravel the complexities of IBD, this targeted therapeutic strategy epitomizes a transformative leap toward individualized pediatric care.
Subject of Research: Pediatric Inflammatory Bowel Disease and Small-Molecule Therapies
Article Title: Small-molecule therapies for pediatric inflammatory bowel disease: toward precision medicine.
Article References:
Chen, Y., Wang, Y., Guo, J. et al. Small-molecule therapies for pediatric inflammatory bowel disease: toward precision medicine. World J Pediatr (2025). https://doi.org/10.1007/s12519-025-01001-6
Image Credits: AI Generated
DOI: 06 December 2025
Tags: challenges in managing pediatric IBDCrohn’s disease and ulcerative colitis in childrenenhancing therapeutic precision in IBDinnovative therapies for chronic diseasesoral bioavailability of small moleculespediatric inflammatory bowel disease treatmentspersonalized healthcare advancementsprecision medicine in pediatric caresmall-molecule drug benefitssmall-molecule therapies for IBDtargeted therapies for inflammatory diseasestransforming pediatric healthcare