Credit: Brett Macaulay, Division of Infectious Diseases, Massachusetts General Hospital
Massachusetts General Hospital (MGH) and Brigham and Women's Hospital (BWH) investigators have developed two approaches to increasing the use of penicillins and cephalosporins – highly effective antibiotics that are not as problematic as many alternatives – in hospitalized patients previously believed to be allergic to penicillin. Their report, which has been published online in the Journal of Allergy and Clinical Immunology, describes how both tested protocols — use of penicillin allergy skin tests or a computerized guideline/decision support tool — safely increased the use of penicillin and penicillin-related antibiotics in inpatients.
"From 10 to 15 percent of hospitalized patients have penicillin allergy in their medical record, but studies have shown that more than 95 percent are not really allergic," explains Kimberly Blumenthal, MD, MSc, of the Division of Rheumatology, Allergy and Immunology, the Medical Practice Evaluation Center, and the Lawrence Center for Quality and Safety at MGH, co-lead and corresponding author of the JACI paper. "We know that over-reporting of penicillin allergies has a negative impact on patient care, as the alternative drugs often used are less effective, more toxic and can both leave patients vulnerable to dangerous C. difficile infection and increase antibiotic resistance in the community. The need to address over-reported penicillin allergy has been widely acknowledged, but how to do that has remained unclear."
"This study offered a unique opportunity to examine what strategy best serves inpatients who have this listed allergy," explains co-lead author Paige Wickner, MD, MPH, of the BWH Division of Rheumatology, Immunology and Allergy and the Department of Quality and Safety.
Over a two-year period — June 2014 to June 2016 — the investigators compared three approaches to treating BWH inpatients who needed antibiotic treatment and had a recorded penicillin allergy. During the first five months, patients on the medical service received standard of care treatment, with testing via either skin test or test dosing conducted only after referral by the primary care team and consultation with an allergy specialist.
During the next seven months, inpatients with a recorded penicillin allergy who needed antibiotic treatment were screened for skin-test eligibility. Those with a history of more serious allergic reactions or those taking drugs that could interfere with skin testing were ineligible, and testing also required consent of the patient and the care team. Patients whose skin test was negative and safely tolerated an oral dose of amoxicillin – a form of penicillin in the same beta-lactam antibiotic class as cephalosporins – were determined not to be allergic.
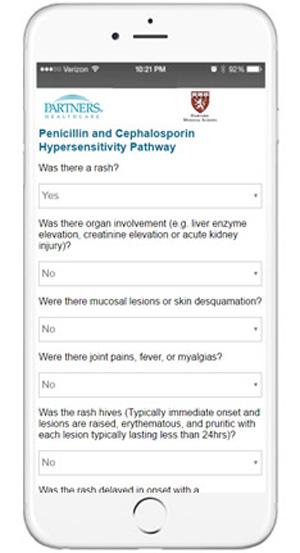
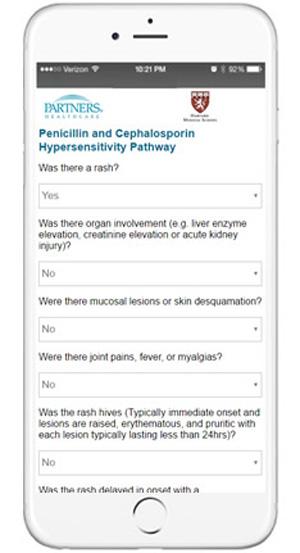
During the third seven-month period, physicians had access to a computerized treatment guideline and decision support system, which – based on details of the reported allergic reaction, such as whether the patient experienced a rash, fever or joint pain – categorized the reaction as follows:
- very low risk – full dose of penicillin or cephalosporin
- low risk – reduced test dose of penicillin or cephalosporin
- medium/high risk – consult with an allergy specialist
- serious reaction – avoid penicillin or cephalosporin.
Due to logistical issues, including schedule coordination and the inability to conduct tests on more than one patient at a time, only 43 of the 179 patients (24 percent) who would have been eligible for skin testing actually had the test. But while that did not result in a significant increase between the standard-of-care and skin-test periods in the overall percentage of those receiving penicillin or cephalosporin, among patients who had the test, the likelihood of receiving the more favorable prescription increased almost six times. In fact, none of the skin-tested patients proved to have a penicillin allergy, and they also had more than double the chance of being discharged with a penicillin or cephalosporin prescription.
During the treatment guideline/decision support period, the likelihood that patients would receive a more favorable antibiotic prescription almost doubled over the standard of care period. Among the providers caring for the 199 medical patients during this period, 112 completed the decision support protocol and there were almost 300 unique webpage views of the guideline, which was accessible both at all hospital desktop computers and through mobile devices connecting to the secure hospital intranet. No adverse reactions occurred during either the standard-of-care or skin-test periods, and only one patient had a mild reaction — an itchy skin rash — to an amoxicillin dose after a negative penicillin skin test during the treatment guideline/decision support period.
Blumenthal notes that the guideline/decision support tool was not integrated into the electronic health record during the study period and that, as the tool becomes more available, it may have an even greater effect on antibiotic prescriptions. The tool has now been adopted at MGH, BWH, Newton-Wellesley Hospital, Brigham and Women's Faulkner Hospital and North Shore Medical Center — all members of Partners HealthCare System. Such a tool also could be useful for hospitals with limited ability to adopt a skin testing protocol or lack of access to staff allergy specialists.
"We found that addressing penicillin allergy by either method could lead to an overall improvement in antibiotic choice for these patients," Blumenthal says. "We don't want to discourage any method of evaluation because even thinking about whether a patient's penicillin allergy is true could lead a provider to make a different management decision. Even here at MGH, we estimated that skin testing all patients with recorded penicillin allergy would be impractical without a significant staff increase or technological guidance."
Wickner adds, "In our Partners system alone, we have more than 200,000 patients who carry this listed diagnosis in the electronic medical record. It is exciting to have safe and effective systems in place to improve the care of these patients when they are hospitalized."
###
Blumenthal is an assistant professor of Medicine at Harvard Medical School (HMS) and the Quality and Safety Officer for Allergy at MGH. Wickner is an instructor of Medicine at HMS and the director of Quality and Safety for Allergy and Immunology at BWH.
Rochelle Walensky, MD, MGH Division of Infectious Disease, is senior author of the JACI paper. Additional co-authors are Shelley Hurwitz, PhD, and Karl Laskowski, MD, MBA, BWH Rheumatology, Allergy, and Immunology; Erica Shenoy, MD, PhD, and, MGH Division of Infectious Disease; Nicholas Pricco, University of Minnesota Medical School; and Andrea Nee, New York Medical College. Support for the study includes the Brigham Care Redesign Incubator and Start Up Program, National Institutes of Health Award (NIH) UL1 TR001102 to the Harvard Clinical and Translational Science Center, NIH grant K01AI125631, and the American Academy of Allergy, Asthma and Immunology Foundation.
Brigham and Women's Hospital (BWH) is a 793-bed nonprofit teaching affiliate of Harvard Medical School and a founding member of Partners HealthCare. Through investigation and discovery conducted at its Brigham Research Institute , BWH is an international leader in basic, clinical and translational research on human diseases, supported by nearly $666 million in funding. For the last 25 years, BWH ranked second in research funding from the National Institutes of Health among independent hospitals. BWH is also home to major landmark epidemiologic population studies, including the Nurses' and Physicians' Health Studies and the Women's Health Initiative as well as the TIMI Study Group, one of the premier cardiovascular clinical trials groups.
Massachusetts General Hospital, founded in 1811, is the original and largest teaching hospital of Harvard Medical School. The MGH Research Institute conducts the largest hospital-based research program in the nation, with an annual research budget of more than $800 million and major research centers in HIV/AIDS, cardiovascular research, cancer, computational and integrative biology, cutaneous biology, human genetics, medical imaging, neurodegenerative disorders, regenerative medicine, reproductive biology, systems biology, photomedicine and transplantation biology. The MGH topped the 2015 Nature Index list of health care organizations publishing in leading scientific journals and earned the prestigious 2015 Foster G. McGaw Prize for Excellence in Community Service. In August 2016 the MGH was once again named to the Honor Roll in the U.S. News & World Report list of "America's Best Hospitals."
Media Contact
Julie Cunningham
[email protected]
617-724-6433
@MassGeneralNews
http://www.mgh.harvard.edu