In the wake of the COVID-19 pandemic, a comprehensive study focusing on colorectal cancer screening practices among privately insured individuals reveals nuanced shifts in diagnostic test utilization, shedding light on broader public health dynamics shaped by unprecedented global disruptions. This detailed investigation highlights not only the overall decline in conventional colorectal screening methods such as colonoscopy and fecal immunochemical testing (FIT), but also an intriguing uptick in the adoption of stool DNA testing, underlining how patient preferences and healthcare delivery modalities have evolved in this challenging landscape.
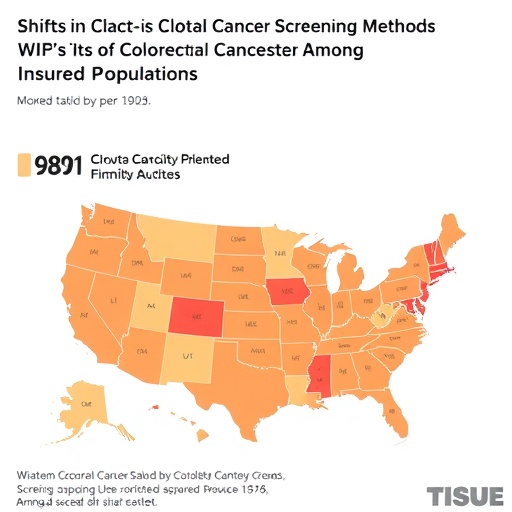
Colorectal cancer remains a leading cause of cancer morbidity and mortality worldwide, and early detection through effective screening is crucial for improving patient outcomes. Traditionally, colonoscopy has been the gold standard for colorectal cancer screening due to its diagnostic accuracy and capacity for simultaneous therapeutic intervention. However, the invasive nature of colonoscopy, coupled with pandemic-induced constraints, likely contributed to its decreased utilization. The study layers socioeconomic factors, geographic disparities, and sex differences to present a multifactorial overview of screening trends, emphasizing that healthcare inequities can be magnified during crises.
Among the requisites that shaped testing patterns was the need to minimize patient exposure to healthcare settings where viral transmission risks were perceived as higher. This acute concern likely propelled a shift towards non-invasive, at-home testing options such as stool DNA tests — which detect cancer-associated genetic material shed in feces. These tests, requiring no direct clinical interaction, gained traction amid a healthcare delivery model increasingly accommodating telehealth and remote patient monitoring. The relative increase in stool DNA testing underpins a broader transition in medical diagnostics towards precision medicine and patient-centric approaches.
The research further delineates differential use patterns stratified by sex, highlighting that male and female patients exhibited variable preferences and access to screening modalities during this period. This sex-based disparity reflects complex interactions between biological risk factors, healthcare-seeking behavior, and systemic barriers, which compounded the pandemic’s impact on routine medical care. Additionally, area-level socioeconomic status emerged as a pivotal determinant, with lower-income populations experiencing steeper declines in colonoscopy and FIT usage, spotlighting the fractured nature of health equity in modern societies.
Geographic variation, particularly urban versus metropolitan residency, painted a nuanced picture of accessibility and uptake. Metropolitan residents, often served by more robust healthcare infrastructure, might ostensibly have better access to diverse screening options; yet pandemic-related service suspensions and resource reallocations challenged these assumptions. Rural and peri-urban populations faced intensified challenges due to limited healthcare facility density and heightened vulnerability to service interruptions, further complicating cancer prevention efforts.
Importantly, the delay or reduction in conventional colorectal screening during the pandemic accentuated concerns regarding the potential for late-stage cancer diagnoses, with downstream implications for treatment complexity, healthcare costs, and survival rates. Screening disruptions questioned the resilience of healthcare systems and the need for adaptable strategies that can safeguard preventive care continuity against future crises.
The integration of molecular diagnostics like stool DNA testing into routine screening protocols exemplifies a technological leap forward, enabling reliable, less-invasive testing that aligns with evolving patient lifestyles and healthcare delivery models. These findings advocate for increased investment in and public health endorsement of such platforms, potentially transforming cancer screening paradigms and improving population-level disease control.
Concurrently, the study underscores the necessity for targeted public health messaging and resource allocation to mitigate socioeconomic and geographic disparities exacerbated during the pandemic. Tailored interventions must address insurance coverage gaps, health literacy challenges, and logistical barriers to ensure equitable screening uptake across diverse demographic groups.
At the intersection of infectious disease management and chronic disease prevention, this research echoes the complex trade-offs enforced by the pandemic’s pressures on healthcare systems. Balancing the urgency of COVID-19 containment with the imperative of maintaining essential services like cancer screening compels innovation in healthcare policy and practice, emphasizing resilience, flexibility, and patient engagement.
Overall, the pandemic-induced shift in colorectal cancer screening practices serves as a bellwether for how healthcare landscapes might evolve in a post-pandemic world. It calls for sustained research, investment, and policy attention to harness technological innovation while addressing persistent disparities — a dual mandate crucial for safeguarding public health amid ongoing and future systemic shocks.
The corresponding author, Dr. Sunny Siddique of Yale, can be contacted for further insights and data inquiries, emphasizing the importance of ongoing collaborative efforts across institutions to monitor, understand, and respond to these evolving trends in cancer diagnostics.
As the medical community continues to assimilate lessons from this period, integrating real-world data and patient feedback will be paramount for refining screening guidelines, optimizing healthcare delivery, and ultimately enhancing cancer prevention strategies worldwide.
Subject of Research: Colorectal Cancer Screening Trends Post-COVID-19 Pandemic Among Privately Insured Individuals
Article Title: [Not specified in the provided content]
News Publication Date: [Not specified in the provided content]
Web References: doi:10.1001/jamanetworkopen.2025.38578
Keywords: Colorectal cancer, Health insurance, Medical treatments, Medical tests, Sex ratios, DNA, Socioeconomics, Geographic regions, COVID-19, Oncology, Patient monitoring
Tags: adoption of stool DNA testingchallenges in colorectal cancer detectioncolorectal cancer screening trendsdisparities in colorectal cancer screeningearly detection of colorectal cancergeographical disparities in health accesshealthcare inequities during crisesimpact of COVID-19 on healthcarepatient preferences in cancer screeningsex differences in cancer screening practicesshifts in diagnostic test utilizationsocioeconomic factors in healthcare