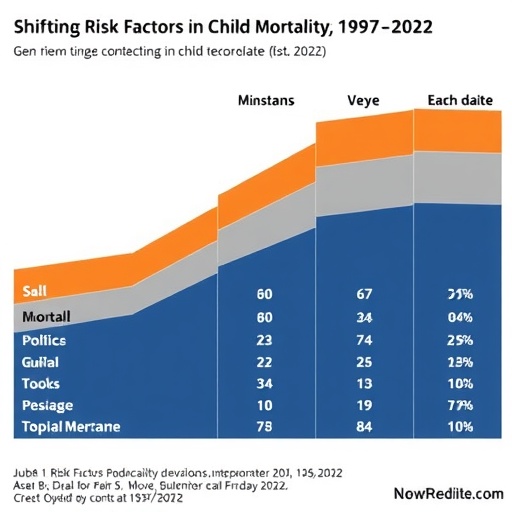
In a groundbreaking new study published in World Journal of Pediatrics, researchers have meticulously analyzed trends in under-five mortality rates across low- and lower-middle-income countries over a 25-year period, from 1997 to 2022. This expansive investigation dissects the shifting contributions of various risk factors contributing to child mortality, offering an unparalleled glimpse into how progress against preventable childhood deaths interplays with evolving socio-economic and health landscapes. The research leverages data from multiple Demographic and Health Surveys (DHS), providing an unprecedented, data-rich perspective on global child health challenges in the current century.
Over the past quarter-century, enormous strides have been made globally in reducing under-five mortality, a crucial indicator of population health and development. However, the researchers underscore that the complex network of risk factors responsible for these deaths has not remained static. Instead, the interplay between biological vulnerabilities, environmental exposures, healthcare access, and socio-economic determinants has evolved, painting a nuanced portrait that policymakers and health practitioners must now contend with. The study reveals that although some traditional factors such as infectious diseases have declined in their mortality burden, emerging challenges and persistent inequities continue to hamper progress, especially in the world’s poorest regions.
The significance of this study lies in its longitudinal approach. By examining DHS data spanning over two decades, the authors can discern patterns that cross national boundaries and reveal commonalities among diverse low- and lower-middle-income countries. The DHS program collects nationally representative data on population, health, and nutrition indicators, allowing this study to harness comprehensive, high-quality information. Such a large-scale comparative analysis enables the extraction of generalizable conclusions about the dynamics driving child mortality trends, moving beyond fragmented snapshots to a global synthesis of risk contributors.
.adsslot_Hv8VSUiskW{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_Hv8VSUiskW{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_Hv8VSUiskW{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
One of the most compelling findings relates to shifting epidemiological patterns underpinning under-five deaths. In the late 1990s, communicable diseases—such as pneumonia, diarrhea, and malaria—dominated the landscape, accounting for a significant share of mortality. Over time, improvements in vaccination coverage, case management, and health system strengthening have curbed many of these infectious killers. However, the relative decline in infectious diseases has exposed the increasing significance of factors such as preterm birth complications, neonatal conditions, and malnutrition. This transition underscores a pressing need to adapt public health strategies from solely combating infections to also addressing neonatal health and chronic nutrition deficits.
In particular, neonatal mortality has emerged as one of the most stubborn barriers in reducing under-five deaths. Neonates—babies aged less than 28 days—now contribute an increasing fraction of overall childhood mortality. This shift reflects both improvements in preventing post-neonatal deaths and the distinct challenges of safeguarding neonates, who are vulnerable to premature birth, asphyxia, and sepsis. The study highlights how prenatal care access, skilled birth attendance, and timely postnatal interventions are critical leverage points in this domain. Yet, inequities in healthcare infrastructure and workforce distribution continue to limit the reach of these essential services in many low-income settings.
Nutritional factors, especially stunting and wasting, maintain a pervasive influence on mortality risk. Although economic development and food security have improved in certain regions, undernutrition remains a stubborn underlying cause of weakened immunity and susceptibility to infections. The analysis reveals that malnutrition’s relative contribution to under-five deaths persists despite some progress in reducing its prevalence. This calls for sustained multisectoral efforts to tackle food insecurity, micronutrient deficiencies, and educational gaps around maternal and child nutrition, emphasizing that nutrition interventions must remain central in child survival programming.
Environmental determinants also play an undeniable role in shaping child mortality risk. Inadequate access to clean water, sanitation, and hygiene (WASH) services perpetuates transmission of diarrheal diseases and parasitic infections, which disproportionately affect young children. Although many countries have made strides in improving these fundamental services, the study finds that millions of children still live in conditions conducive to preventable infections. Furthermore, the mounting impact of climate change and urbanization introduces new and complex health risks, requiring more adaptive, resilient public health infrastructure.
Socioeconomic disparities persist as a defining characteristic of under-five mortality patterns. The research demonstrates that children from the poorest quintiles consistently experience significantly higher death rates than their wealthier counterparts. Inequities in access to nutrition, healthcare, education, and sanitation create a compounding disadvantage that intensifies vulnerability. Notably, the study’s data-driven approach quantifies how risk factors disproportionately affect marginalized populations, underscoring the imperative to design equity-focused interventions that close health gaps and address structural determinants of poverty.
A crucial dimension of this study is its focus on the relative contributions of individual risk factors rather than solely mortality rates. This analytic nuance allows policymakers to identify which interventions may yield the greatest impact in specific country contexts by prioritizing the most influential determinants of child deaths. For example, in settings where infectious diseases have dwindled, scaling up neonatal care and nutritional programs may be the most efficient investment. Conversely, in regions still grappling with high infectious burdens, intensifying immunization and infection control remains vital.
The methodological rigor of the study further enhances its credibility. Using advanced statistical decomposition techniques, the authors disaggregate mortality changes into component risk drivers over time. This quantitative precision provides clarity on complex epidemiological shifts that would otherwise remain obscured within aggregate mortality statistics. Additionally, the broad geographic scope and harmonization across numerous DHS datasets boost the external validity and relevance of insights for global health stakeholders and donors.
Importantly, this research holds profound implications for the Sustainable Development Goals (SDGs), particularly SDG 3, which aims to end preventable deaths of newborns and children under 5 by 2030. The findings affirm that despite notable global progress, reaching such ambitious targets demands agile responses to changing risk landscapes. It calls for integrated policies that combine disease control with maternal and neonatal health, nutrition, WASH, and social protection programs. The research highlights the necessity of cross-sector collaboration and innovative financing to sustain and accelerate declines in under-five mortality.
Furthermore, the temporal span of this work captures the health impacts of diverse global trends, including economic crises, conflicts, and recent pandemics such as COVID-19. Disruptions in health services during the pandemic have threatened gains and exposed vulnerabilities in health systems. By providing a baseline of risk factor evolution, this study equips policymakers to better understand how shocks exacerbate child mortality and where resilience must be bolstered in post-pandemic recovery strategies.
Technological advancements feature as an undercurrent throughout the study’s analyses. From the scaling up of vaccines such as pneumococcal and rotavirus to innovations in newborn care practices, technology has been a key enabler of mortality reduction. However, bridging the “last mile” to reach the most underserved populations remains a formidable challenge that requires innovative delivery models, digital health solutions, and community engagement strategies to expand coverage and adherence.
In conclusion, this expansive analysis sheds vital light on the fluid, multifactorial nature of under-five mortality reductions in low- and lower-middle-income countries over the past 25 years. By parsing the evolving contributions of risk factors, it charts a path for tailored, data-driven interventions that reflect the realities of today’s global child health environment. As the world seeks to fulfill its promise to every child’s right to life and health, these insights will be indispensable in guiding effective policy, funding, and programmatic decisions that save millions of young lives.
Subject of Research: Under-five mortality risk factors and their changing contributions in low- and lower-middle-income countries from 1997 to 2022.
Article Title: Changes in the contributions of risk factors to under-five mortality in low- and lower-middle-income countries (1997–2022): an analysis of Demographic and Health Survey data.
Article References:
Kefale, B., Jancey, J., Gebremedhin, A.T. et al. Changes in the contributions of risk factors to under-five mortality in low- and lower-middle-income countries (1997–2022): an analysis of Demographic and Health Survey data. World J Pediatr 21, 502–514 (2025). https://doi.org/10.1007/s12519-025-00912-8
Image Credits: AI Generated
DOI: 10.1007/s12519-025-00912-8 (May 2025)
Tags: child mortality trends 1997 to 2022Demographic and Health Surveys analysisenvironmental exposures affecting child healthevolving child mortality risk factorsglobal health challenges in child mortalityhealthcare access and child mortalityinfectious diseases and child deathslow-income countries child mortality ratesprogress in reducing childhood deathsrisk factors in under-five mortalitysocio-economic determinants of child healthtraditional vs emerging health risks