Credit: CHEST
GLENVIEW, IL, February 13, 2017 – Sepsis is a major public health problem and the focus of national quality measures and performance improvement initiatives. Understanding what is happening with sepsis rates and outcomes is thus an area of great importance. However, tracking sepsis rates and outcomes is challenging because it is a heterogeneous syndrome without a definitive "gold standard" test. In the February issue of CHEST, investigators compared the effectiveness of claims-based surveillance using ICD-9 codes with clinical-based data and specific diagnostic parameters. Their findings suggest that surveillance based on clinical criteria is a more reliable way to track cases of septic shock.
"Our results underscore the challenges in tracking sepsis and septic shock using diagnosis billing codes, which is the current method typically used for epidemiologic studies as well as quality measures. We show, however, that an alternative surveillance method using clinical data is feasible and may provide more reliable estimates of trends over time," explained co-lead investigator Chanu Rhee, MD, MPH, Department of Population Medicine, Harvard Medical School/Harvard Pilgrim Health Care Institute and Division of Infectious Diseases, Brigham and Women's Hospital, Boston, MA.
Researchers examined data from 27 academic hospitals between 2005-2014 and looked for cases of septic shock using two different methods: claims data and clinical data. For claims-based surveillance, they located cases with septic shock-related ICD-9 billing codes. For clinical surveillance, they looked for patients who received concurrent vasopressors, blood culture orders, and antibiotics. When compared, they showed the sensitivity was higher for the clinical criteria than for the claims (74.8 percent versus 48.3 percent) relative to medical record reviews, but positive predictive value was comparable (83 percent versus 89 percent).
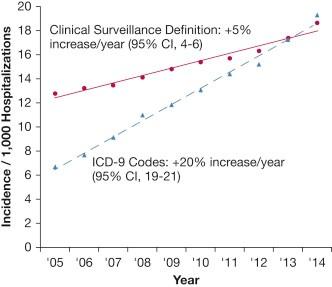
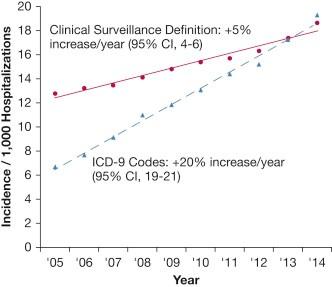
The greatest differences the team found came when looking at septic shock trends over time. Investigators found that with clinical data, septic shock cases rose from 12.8 to 18.6 per 1,000 hospitalizations, while mortality declined from 54.9 percent to 50.7 percent. Meanwhile, the results from ICD-9 codes show a much larger jump, from 6.7 to 19.3 cases per 1,000 hospitalizations, while mortality decreased from 48.3 percent to 39.3 percent.
"The incidence of patients with discharge codes or clinical markers indicative of treated septic shock steadily rose during the 10-year surveillance period, and in-hospital mortality for this population declined," stated Dr. Rhee. "The magnitude of these trends was considerably less when using clinical data compared with claims codes. Clinician record reviews suggested that clinical surveillance definitions for septic shock provide greater sensitivity and comparable positive predictive value than billing codes."
While both datasets showed an increase in cases and a decline in mortality, the clinical numbers suggest this shift has been much less dramatic than previously believed. "Tracking trends in septic shock incidence and outcomes is critical to informing the allocation of health care resources and interpreting the impact of sepsis prevention and treatment initiatives," said Dr. Rhee. "However, it remains unclear whether claims-based reports of dramatic rises in sepsis and septic shock incidence and declining case fatality rates reflect more infections, better recognition, more aggressive treatment, and/or more comprehensive coding."
Investigators also observed that other factors may influence the statistics about septic shock mortality. As more patients opt to leave the hospital setting for end-of-life care at a hospice, the number of hospital deaths from septic shock is declining. "Not accounting for this evolving societal preference can exaggerate the overall impression of improving outcomes," noted Dr. Rhee.
While septic shock continues to be an important area of focus for practitioners and public health experts, tracking clinical data may prove to be a better way to accurately observe septic shock trends. "The imperfect sensitivity of codes as well as our clinical surveillance definition suggest that both methods may still underestimate the true burden of septic shock," concluded Dr. Rhee. "However, surveillance-based clinical data may allow for more reliable estimates of septic shock burden and trends compared with administrative data."
###
Media Contact
Andrea Camino
[email protected]
224-521-9513
@elseviernews
https://www.elsevier.com/