Specific changes in our movement patterns can be indicators of several health problems: For instance, decrease in strength often correlates with risk of falls, mild cognitive impairment, depression, sleep problems, respiratory problems, cardiac arrhythmias and increasing myocardial weakness or worsening of a COVID-19 infection. In older individuals, systematic detection of such changes could help identify chronic diseases such as dementia, Parkinson’s disease, or heart disease at an early stage. These age-related health problems are often discovered late, and their progression is usually difficult to assess objectively.
Credit: © NeuroTec/Nature Scientific Reports, Creative Commons Licence
Specific changes in our movement patterns can be indicators of several health problems: For instance, decrease in strength often correlates with risk of falls, mild cognitive impairment, depression, sleep problems, respiratory problems, cardiac arrhythmias and increasing myocardial weakness or worsening of a COVID-19 infection. In older individuals, systematic detection of such changes could help identify chronic diseases such as dementia, Parkinson’s disease, or heart disease at an early stage. These age-related health problems are often discovered late, and their progression is usually difficult to assess objectively.
An interdisciplinary research team led by Tobias Nef of the ARTORG Center for Biomedical Engineering Research, and Professor Emeritus of Cardiology Hugo Saner of the University of Bern and Bern University Hospital, now shows how large-scale, sensor-based health monitoring could tackle these problems. The researchers combined a variety of everyday activity and behavior patterns measured by sensors in the homes of elderly study participants helping them to create a summary picture. “We used non-contact sensors at home to create an extensive collection of digital measures that capture broad parts of daily life, behavior and physiology, in order to identify health risks of older people at an early stage,” explains study first author and postdoctoral researcher Dr. Narayan Schütz. This may benefit early detection as well as foster development of personalized treatments and research into new therapeutic approaches and drugs. The study was published in npj Digital Medicine.
Reliable system accepted by seniors
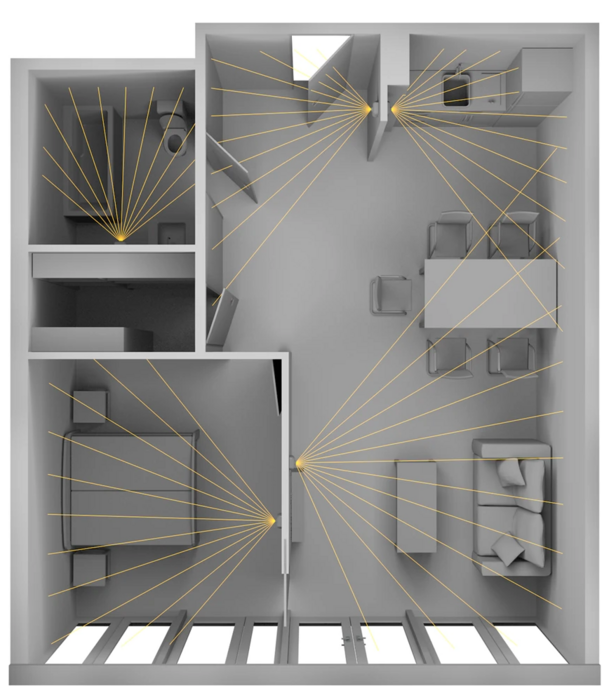
The researchers initially collected 1,268 health parameters using non-interaction sensors particularly tailored to the senior demographic. The deployed system consists of simple, contactless motion sensors in each room, a bed sensor under the mattress, and door sensors on the front door and on the refrigerator. Connected to a base station, the system analyzes the registered motion signals and can inform relatives or an alarm center in the event of problems or emergencies – such as when a person does not return to bed at night. The researchers then evaluated the data collected in this way using machine learning approaches.
“We were able to show that such a systems approach – in contrast to the common use of a few health metrics – allows to detect age-relevant health problems such as cognitive impairment, fall risk or frailty surprisingly well,” says Tobias Nef, Professor of Gerontechnology and Rehabilitation at the ARTORG Center and co-last author of the study. Compared to wearable devices, this sensor-based home monitoring approach was perceived well among seniors: As the interdisciplinary research group led by Tobias Nef and Hugo Saner was able to prove in a scientific collaboration of computer science, behavioral research and medicine spanning more than ten years, older test subjects in Switzerland found the daily operation of mobile devices rather cumbersome, and some were unable to handle them at all due to dexterity or cognitive problems. In particular, older adults above 80 years of age clearly preferred a zero-interaction system such as the one used in the study.
In addition, data protection and privacy are prioritized: “To ensure privacy and data protection on a technical level, the highest Swiss and European medical data security standards are applied”, Narayan Schütz points out. To secure privacy, the deployed sensors also do not record sound or video and their installation is entirely voluntary – both aspects that the study participants appreciated.
Great potential
The evaluation and combination of the large amount of everyday health data also offers the potential to identify possible new aging-relevant digital biomarkers: “For example, we found indications that fall risk could significantly depend on certain sleep parameters,” explains Tobias Nef.
Prof. Hugo Saner, who was responsible for clinical data collection and is co-last author of the study, assesses the clinical relevance of the results: “Such a system marks a milestone in early detection of worsening health for seniors living alone into old age. We assume that it can make a significant contribution to enabling older people to live at home for as long as possible by delaying hospital admissions and transfers to nursing institutions or, in the best case, even avoiding them.” According to the researchers, better early detection, and personalized treatment of typical diseases of old age would not only help older people achieve better health, but also reduce healthcare costs.
DOI
10.1038/s41746-022-00657-y




