In the relentless battle against life-threatening fungal infections, a groundbreaking advance has emerged that could redefine the future of antifungal therapy. A team of researchers has engineered a novel polymer-based delivery system that not only enhances the efficacy of existing antifungal drugs but also dramatically reduces their toxicity. This innovative approach involves the design of a synthetic polymer mimicking host defense peptides, which self-assembles into micelles capable of encapsulating and delivering a second antifungal agent with remarkable precision, achieving unprecedented temporal and spatial consistency in drug release.
Systemic fungal infections pose a significant clinical challenge worldwide, often leading to high mortality rates despite the availability of potent antifungal agents. One of the primary obstacles in treating these infections lies in the distinct in vivo pharmacokinetic profiles of two-drug regimens, which hamper their synergistic potential. By addressing this pharmacological disconnect, the research team has developed a strategy that synchronizes drug delivery, ensuring both agents act in concert at the site of infection.
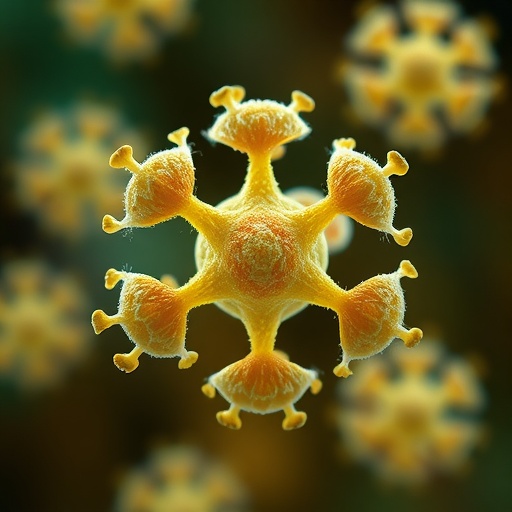
At the heart of this breakthrough is the polymer designed to emulate host defense peptides—natural molecules intrinsic to the immune system renowned for their broad-spectrum antimicrobial properties and ability to disrupt microbial membranes. These synthetic peptides self-assemble into nanoscale structures called micelles, which can encapsulate amphotericin B (AmB), a potent antifungal drug known for its efficacy but also its significant toxicity. The resulting AmB-loaded micelles (AmBmicelles) exhibit a capacity for slow and controlled drug release, mitigating the adverse effects commonly associated with AmB therapy.
One of the most compelling attributes of these AmBmicelles is their selective targeting of fungal pathogens. This specificity is attained through charge interactions between the cationic polymer micelles and the negatively charged fungal membranes, which facilitates binding and subsequent drug delivery at the infection site without affecting mammalian cells. This targeted approach not only enhances the therapeutic index of AmB but also reduces collateral damage to host tissues.
In preclinical mouse models of systemic candidiasis and cryptococcal meningitis, AmBmicelles demonstrated a remarkable ability to improve survival rates by 67 to 100 percent compared to the current gold standard therapies, including AmBisome and the combined treatment of AmBisome with 5-flucytosine. These results suggest that the micellar delivery system can significantly enhance the clinical outcomes of antifungal therapy, especially in drug-resistant infections that remain a persistent global health threat.
The mechanistic underpinnings of this synergistic effect are rooted in the dual action of the polymer and AmB. While AmB disrupts fungal cell membranes through ergosterol binding, the polymer mimetic itself exhibits anti-fungal activity by perturbing membrane integrity. When combined in the micellar assembly, these actions complement and potentiate each other, leading to comprehensive fungal eradication that surpasses the efficacy of either agent alone.
Furthermore, the slow release kinetics of AmB from the micelles prolong drug exposure at the infection site, maintaining effective concentrations for extended periods. This controlled release not only maximizes therapeutic effects but also mitigates the nephrotoxicity and infusion-related reactions traditionally associated with AmB, thereby vastly extending its therapeutic window in vivo.
Another pivotal advantage of the AmBmicelles lies in their ability to overcome the pharmacokinetic limitations that have hindered previous combinatorial antifungal therapies. The synchronized delivery ensures that both the polymer and AmB reach infectious foci simultaneously, thereby amplifying their synergistic potential and suppressing fungal proliferation more efficiently than staggered drug administration.
The research also underscores the versatility of this platform technology, which could be adapted to deliver other antifungal agents or even antibiotics, thereby broadening its impact on managing diverse infectious diseases. Given the rising tide of antimicrobial resistance, this innovation signals a crucial step forward in developing next-generation combination therapies that are both potent and safe.
Importantly, the AmBmicelles demonstrated excellent biocompatibility and stability in physiological environments, an essential criterion for clinical translation. The polymeric micelles maintained their structural integrity and drug-loading capacity in complex biological fluids, indicating their robustness for systemic administration.
The design process involved sophisticated polymer synthesis techniques to precisely control the amphipathic balance and charge density necessary for self-assembly and targeted interaction with fungal membranes. Such customization ensures not only effective drug encapsulation but also optimal pharmacodynamic performance.
In addition to efficacy and safety, scalability and manufacturability of this micellar system present practical advantages. The polymer synthesis is amenable to large-scale production, offering a feasible pathway for clinical development and eventual commercialization, a critical step towards addressing the urgent unmet needs in antifungal therapeutics.
Moving forward, the researchers aim to advance these promising findings into clinical trials to evaluate the safety and efficacy of AmBmicelles in humans. Such trials will be pivotal in confirming the potential of this technology to transform antifungal treatment paradigms and save countless lives threatened by invasive fungal diseases.
This research epitomizes the convergence of materials science, pharmacology, and infectious disease biology, illustrating how bioinspired engineering can unlock novel therapeutic avenues. By harnessing the inherent antimicrobial strategies of the immune system and pairing them with advanced drug delivery technologies, the study sets a new benchmark in combating recalcitrant fungal infections.
As the global health community grapples with increasing fungal resistance and limited therapeutic options, the emergence of AmBmicelle technology instills hope for safer and more effective treatment regimens. This interplay between polymer chemistry and antifungal pharmacotherapy highlights the transformative potential of interdisciplinary innovation in addressing some of the most stubborn and deadly infectious diseases of our time.
Subject of Research: Combinatorial antifungal therapy using a host defense peptide mimic polymer forming delivery micelles for enhanced amphotericin B efficacy.
Article Title: Effective combinatorial antifungal therapy using a host defense peptide mimic that self-assembles into delivery micelles.
Article References: Liu, L., Zhou, M., Xiao, X. et al. Effective combinatorial antifungal therapy using a host defense peptide mimic that self-assembles into delivery micelles. Nat Biotechnol (2026). https://doi.org/10.1038/s41587-025-02930-3
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41587-025-02930-3
Tags: antifungal therapy innovationsantimicrobial properties of synthetic peptidesenhanced antifungal drug efficacyhost defense peptide mimicsnanoscale drug delivery structuresnovel antifungal strategiespolymer-based drug delivery systemsprecision drug release mechanismsreduced toxicity in antifungal treatmentsself-assembling peptide micellessynergistic drug regimens for fungal infectionssystemic fungal infection challenges