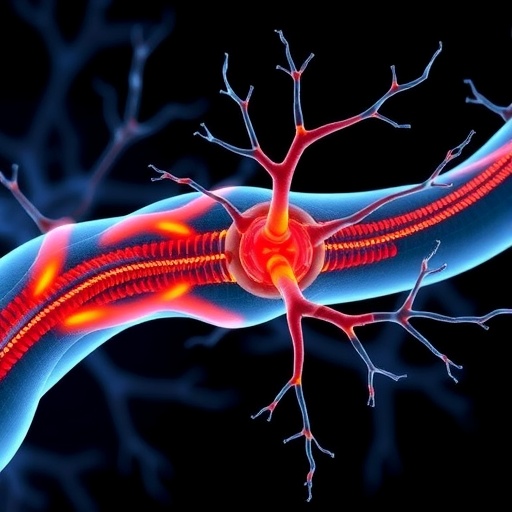
A groundbreaking discovery by scientists at Wake Forest University School of Medicine, in collaboration with Weill Cornell Medicine, sheds critical light on a pervasive and painful complication faced by cancer patients undergoing chemotherapy: chemotherapy-induced peripheral neuropathy (CIPN). This debilitating condition, characterized by numbness, tingling, and excruciating pain predominantly in the hands and feet, has long mystified researchers and clinicians alike. Until now, the molecular mechanisms fueling nerve damage and the resultant neuropathic pain remained elusive, severely limiting effective preventative or therapeutic options.
Chemotherapy drugs such as paclitaxel—a cornerstone treatment for many malignancies—though lifesaving, frequently precipitate this insidious neuropathy. Nearly 50% of patients treated with such agents endure symptoms severe enough to necessitate modifications or discontinuation of chemotherapy, thereby jeopardizing their cancer battle. The conundrum lies in the absence of clearly understood cellular targets driving this neurotoxicity. Addressing this knowledge gap, the research team employed an established murine model that faithfully recapitulates the sensory impairments and inflammatory milieu observed in human CIPN.
Their investigative focus converged on a cellular stress sensor known as inositol-requiring enzyme 1 alpha (IRE1α), localized within immune cells. IRE1α functions as a sentinel of endoplasmic reticulum (ER) stress—conditions that disrupt protein folding homeostasis—triggering unfolded protein responses (UPR). Notably, aberrant activation of this pathway has been implicated in various chronic inflammatory and neurodegenerative diseases, but its role in chemotherapy-associated neuropathy was previously uncharted territory.
Through meticulous experimentation, the researchers demonstrated that chemotherapy initiates a robust activation of the IRE1α pathway within leukocytes, particularly influencing inflammatory cascades. This immune cell-intrinsic ER stress response orchestrates a proinflammatory state that culminates in nerve injury and heightened pain sensation. Critically, interventions that genetically ablated or pharmacologically inhibited IRE1α signaling in these immune populations effectively abrogated the development of neuropathic symptoms in mice. These findings implicate IRE1α as a pivotal driver of chemotherapy-elicited peripheral nerve inflammation and damage.
Translating these murine insights to humans, the team conducted a prospective clinical study involving patients treated for gynecological cancers at the National Cancer Institute-designated Comprehensive Cancer Center affiliated with Atrium Health Wake Forest Baptist. Blood samples harvested before and after chemotherapy revealed a direct correlation between elevated IRE1α activation in immune cells and the emergence of severe neuropathy symptoms. This direct link emphasizes IRE1α not only as a mechanistic culprit but also a promising biomarker for predicting CIPN susceptibility in cancer patients.
The prospect of therapeutically targeting IRE1α opens novel avenues for mitigating chemotherapy-induced neuropathic pain without compromising anti-cancer efficacy. The current landscape lacks FDA-approved agents that specifically prevent or reverse CIPN, leaving patients vulnerable to this distressing side effect that detrimentally affects quality of life. By illuminating the IRE1α axis as a master regulator in this pathological process, this study paves the path toward precision medicine approaches tailored to individual neuropathy risk profiles.
Intriguingly, IRE1α inhibitors are presently under clinical evaluation for enhancing chemotherapy’s anti-tumor action, including against regimens employing paclitaxel. This convergence offers a tantalizing dual-benefit therapeutic strategy: simultaneously augmenting malignancy control while shielding peripheral nerves from insult. Future clinical trials designed to evaluate the safety, tolerability, and efficacy of IRE1α blockade for neuropathy prevention will be paramount in revolutionizing supportive care in oncology.
Beyond chemotherapy-induced neuropathy, this discovery may hold broader implications across diverse neuropathic pain syndromes where ER stress and immune dysregulation intersect. Chronic pain conditions associated with nerve damage pose formidable treatment challenges, often resistant to conventional analgesics. The elucidation of leukocyte-intrinsic ER stress mechanisms contributing to neuroinflammation thus enriches the fundamental understanding of pain pathophysiology.
Dr. E. Alfonso Romero-Sandoval, the study’s corresponding author and professor of anesthesiology at Wake Forest University School of Medicine, underscored the transformative potential of these findings. He emphasized that delineating the immune cell stress responses fueling nerve damage marks a strong step forward in developing patient-tailored interventions. The ability to predict which patients are at heightened risk for neuropathy before onset would profoundly impact clinical decision-making, enabling prophylactic or early therapeutic measures.
The study’s rigorous scientific methodology, incorporating both genetic manipulation and pharmacological modulation in animal models alongside translational human data, reinforces its validity and promising clinical relevance. This integrative bench-to-bedside approach exemplifies contemporary biomedical research striving to unravel complex treatment-limiting toxicities.
Funded by prestigious entities including the National Cancer Institute, National Institute of Neurological Disorders and Stroke, and the U.S. Department of Defense, this research exemplifies collaborative efforts to surmount the adverse effects of cancer therapies. Wake Forest University School of Medicine, renowned for its commitment to innovation through over 1,000 clinical trials nationwide, houses the NCI-designated Comprehensive Cancer Center pivotal in advancing cancer care for more than half a century.
As this field advances, the scientific community eagerly anticipates expanded clinical studies to validate IRE1α’s utility as a biomarker and therapeutic target. Should these endeavors prove successful, millions of cancer patients worldwide stand to benefit from interventions that preserve neural integrity and wellbeing, dramatically enhancing survivorship experience.
In summary, by uncovering the central role of leukocyte-intrinsic ER stress responses mediated by IRE1α in chemotherapy-induced peripheral neuropathy, this pioneering work heralds a new horizon in oncology supportive care. Moving forward, targeting cellular stress pathways in immune cells represents a compelling strategy to alleviate one of the most vexing side effects undermining cancer treatment success. This discovery may ultimately translate to tangible improvements in patient quality of life, symptom management, and therapeutic adherence throughout the cancer journey.
Subject of Research: Chemotherapy-induced peripheral neuropathy and immune cell ER stress mechanisms
Article Title: Leukocyte-intrinsic ER stress responses contribute to chemotherapy-induced peripheral neuropathy
News Publication Date: 29-Oct-2025
Web References:
Science Translational Medicine Article DOI
Keywords: Chemotherapy, Cancer treatments, Neuropathic pain, Peripheral nervous system, Immune response, Neurotoxicity, Pain
Tags: cancer treatment side effectschemotherapy-induced peripheral neuropathyeffective prevention of chemotherapy side effectsendoplasmic reticulum stress in neuropathyinflammatory response in chemotherapyIRE1α role in neurotoxicitymechanism of nerve damage in chemotherapyneuropathic pain management strategiespaclitaxel and nerve painsensory impairments in cancer patientstherapeutic targets for CIPNWake Forest University School of Medicine research