In a groundbreaking discovery that promises to reshape our understanding of autoimmune diseases, researchers from Washington University School of Medicine in St. Louis, alongside their colleagues from the Perelman School of Medicine at the University of Pennsylvania, have identified a previously overlooked protein that plays a crucial role in immune system regulation. This development is particularly significant for diseases like STING-associated vasculopathy with onset in infancy (SAVI), which afflicts a minuscule portion of the population and poses severe health risks, including premature death.
For years, scientists have sought to unravel the complex processes behind autoimmune disorders, which affect over 15 million people in the United States alone. These ailments arise from a hyperactive immune response in which the body mistakenly identifies non-threatening agents as harmful, causing an unnecessary assault on healthy tissues. The research team’s latest findings shine new light on one of the pivotal steps in this chain of miscommunication that has baffled experts for decades.
The researchers’ paper, published in the prestigious journal Cell, unveils how a protein, ArfGAP2, is instrumental in orchestrating the final stages of cytokine release—the signaling molecules essential for immune responses. More critically, the role of ArfGAP2 as a conductor of this process was previously unrecognized, making this discovery a significant addition to the known pathways regulating immune function. This revelation could set the stage for novel therapeutic approaches aimed at mitigating the adverse effects of autoimmune disorders.
SAVI itself is a rare condition that usually emerges within the first year of life, with an incidence rate estimated at only one in one million births. The illness arises from a mutation in the STING protein, which normally acts as a guardian of cellular health, alerting the immune system to the presence of viral DNA. In patients suffering from SAVI, this protein is hyperactive, resulting in chronic inflammation and tissue damage primarily affecting the lungs and limbs. The implications of this dysfunction extend beyond SAVI, offering insights into more prevalent autoimmune conditions that similarly involve dysregulated immune responses.
Examining rare diseases can provide extraordinary opportunities to decipher the underlying biological mechanisms that govern more common health issues. By studying the specific mutations in STING that lead to SAVI, the research team has uncovered potential therapeutic targets that may not only help in this rare disorder but could also be translated to other inflammatory diseases characterized by cytokine overproduction. Indeed, cytokine storms—excessive immune responses seen in conditions such as COVID-19—are a prime example of disorders that could benefit from this research.
Through rigorous experimental studies, the researchers demonstrated that ArfGAP2 plays a dual role: not only does it contribute to the synthesis of immune proteins but it also aids in their release from the cells. This multifaceted functionality provides a pathway toward exploring how modulators of ArfGAP2 could be harnessed to dampen overactive immune signaling. Given the devastating outcomes associated with uncontrolled immune responses, the findings present a pivotal shift in the paradigm of immunotherapy.
In their experiments, the team utilized mouse models genetically modified to mimic the STING mutations seen in SAVI patients. They confirmed that the absence of ArfGAP2 resulted in a cessation of the destructive immune attacks commonly observed in SAVI. The metaphor likening ArfGAP2 to a train conductor gives an accessible understanding of the protein’s function in directing the release of immune molecules—akin to ensuring that each train (cytokine) reaches its intended destination within the body.
As researchers continue to investigate the intricacies of immune responses and the roles played by various proteins, ArfGAP2 stands out as a focal point for future studies. The goal of translating laboratory findings to clinical applications is now within reach as more evidence accumulates about how specific proteins can modulate immune system behavior. Collaborations across institutions further exacerbate the potential for breakthroughs that could transform the landscape of autoimmune disease treatment.
This innovative research underscores the necessity for continued exploration into the complex web of interactions that comprise our immune system. With strategic funding and support from entities like the National Institutes of Health, further advancements in understanding and treating disorders tied to dysregulated immune responses remain promising. The commitment to unraveling the underlying mechanisms of immune-related diseases will hopefully lead to effective interventions that can change the lives of millions affected by such conditions.
In summary, the discovery of the ArfGAP2 protein’s role in immune signaling offers an exciting new avenue for therapeutic development that may well revolutionize how we approach autoimmune diseases. The implications reach far beyond the confines of SAVI, propelling research into more widespread inflammatory conditions that impact global health. As the scientific community digests these findings, the next steps will involve deeper investigations aimed at elucidating the broader ramifications of this protein’s role in immune system regulation.
Subject of Research: Immune Response in Autoimmune Diseases
Article Title: ArfGAP2 Promotes STING Proton Channel Activity, Cytokine Transit, and Autoinflammation
News Publication Date: 12-Feb-2025
Web References: Cell Journal Article
References: The research paper referenced herein
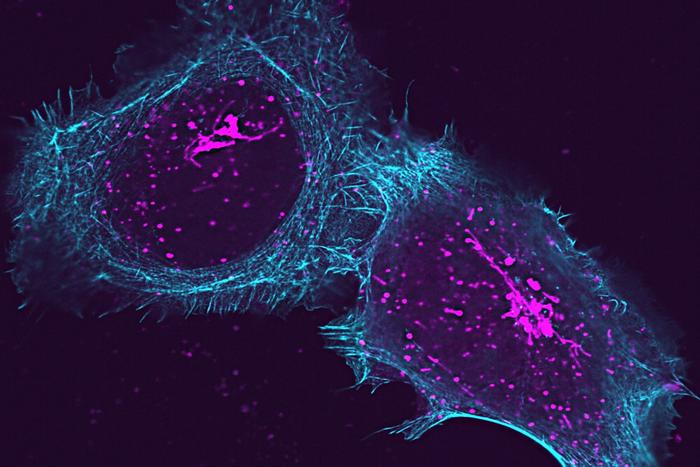
Image Credits: Credit: David Kast
Keywords: Autoimmune disorders, cytokines, immune response, STING protein, ArfGAP2, SAVI, chronic inflammation, immunotherapy.
Tags: advances in immunology studiesautoimmune disease researchcytokine release mechanismsgroundbreaking medical researchhealth risks of autoimmune conditionsimmune system regulationimplications for rare autoimmune diseasesprotein function in autoimmune disordersrole of ArfGAP2 in immunitySTING-associated vasculopathy discoveryunderstanding hyperactive immune responsesWashington University School of Medicine