In the intricate realm of neonatal intensive care, the management of severe bronchopulmonary dysplasia (BPD) remains one of the most challenging frontiers. As survival rates of extremely preterm infants continue to improve, the incidence of chronic lung disease such as grade 3 bronchopulmonary dysplasia (G3-BPD) has paradoxically become a more pressing clinical concern. A recent study by Zierk and colleagues, published in the Journal of Perinatology in 2025, sheds critical light on a previously underexplored aspect of neonatal respiratory care: the predictors of extubation success within this vulnerable population. Their findings point to the respiratory severity score (RSS) as a potent marker, potentially revolutionizing how clinicians approach the delicate transition from invasive ventilation.
Bronchopulmonary dysplasia, particularly at its most severe grade, signals relentless pulmonary insufficiency and profound structural alteration within the preterm infant’s lungs. Despite advances in ventilation strategies and pharmacotherapy, infants with G3-BPD often require prolonged mechanical ventilation, which itself carries substantial risks including ventilator-associated injury, infection, and neurodevelopmental delays. The process of extubation—removal of the endotracheal tube to allow spontaneous breathing—therefore warrants utmost precision. Historically, predicting which infants will succeed after extubation has eluded neonatologists, leading to repeated failures and subsequent reintubations, each episode compounding the infant’s fragile condition.
The respiratory severity score (RSS), previously validated in the context of early respiratory distress syndrome among premature neonates, quantifies the cumulative burden of oxygen requirement and ventilation settings. This composite score serves as an index of the infant’s respiratory workload and pulmonary compromise. Zierk et al. veered into new territory by investigating the RSS’s role in a cohort of infants with established severe BPD, thereby shifting focus from initial respiratory distress to chronic disease management. This approach underscores a nuanced understanding: while the pathophysiology of early respiratory failure contrasts with progressive pulmonary remodeling in BPD, the RSS may nevertheless retain prognostic relevance.
.adsslot_wh7RxlS0sb{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_wh7RxlS0sb{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_wh7RxlS0sb{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
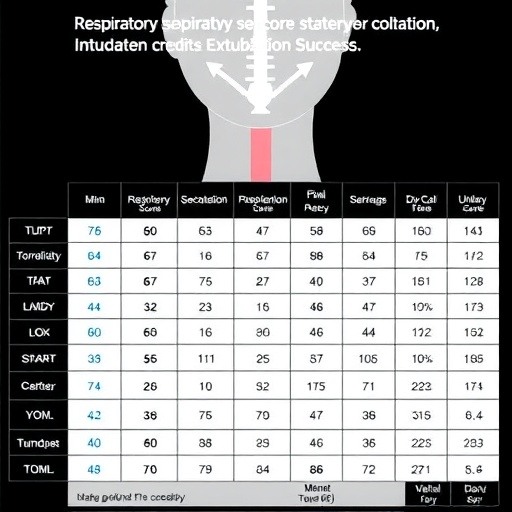
In their study, the researchers meticulously evaluated a cohort of infants diagnosed with grade 3 BPD, critically analyzing the relationship between pre-extubation RSS values and subsequent extubation outcomes. The cohort was derived from a tertiary neonatal intensive care unit with stringent inclusion criteria to ensure homogeneity of the sample and eliminate potential confounding clinical variables. This rigorous methodology provided a robust platform to test the hypothesis that RSS could serve as a reliable predictor of extubation success in severe bronchopulmonary dysplasia.
Their analysis revealed a compelling trend: lower RSS values immediately preceding extubation correlated strongly with successful liberation from mechanical ventilation. Conversely, elevated RSS values portended extubation failure, necessitating timely reconsideration of extubation readiness or augmented respiratory support strategies. These findings offer a critical quantitative tool to supplement clinician judgment and subjective assessment, which have traditionally dominated extubation decision-making processes. By integrating RSS into extubation protocols, neonatal teams could reduce the incidence of failed extubations, thereby improving patient outcomes and optimizing resource utilization in intensive care settings.
One of the remarkable aspects of Zierk and colleagues’ work is the potential applicability of the RSS not only as a prognostic score but also as a dynamic monitoring metric. Given the chronic and often fluctuating trajectory of pulmonary function in G3-BPD, serial RSS measurements could enable earlier detection of deteriorations or improvements, informing both ventilation management and the timing of extubation trials. This dynamic framework holds promise for personalized respiratory care, tailoring interventions to the evolving needs of each infant rather than relying solely on static clinical snapshots.
Moreover, the implications of this study extend beyond mere respiratory parameters. Successful extubation in infants with severe BPD is increasingly recognized as a pivotal milestone with reverberations across neurodevelopmental domains. The reduction of invasive ventilation duration may mitigate the risk of ventilator-induced lung injury and systemic inflammation, both implicated in adverse neurodevelopmental outcomes. Therefore, the establishment of reliable predictive tools like the RSS can indirectly foster improved long-term quality of life for these infants as they progress through critical windows of brain growth and development.
In the broader scientific context, this research resonates with a growing movement towards precision medicine in neonatology. Traditionally, management protocols for BPD have been largely protocol-driven and uniform, despite known heterogeneity in disease presentation and response. The incorporation of quantifiable tools such as RSS heralds a transition towards data-driven decision-making, where individualized patient profiles inform therapeutic choices. Such advancements align with global trends in pediatrics and critical care aimed at enhancing efficacy while minimizing iatrogenic harms.
The study also highlights enduring gaps in our understanding of BPD pathophysiology and the multifactorial influences on respiratory outcomes. While the RSS provides a snapshot of oxygenation and ventilator settings, it does not capture the complex interplay of pulmonary vascular disease, airway inflammation, or parenchymal remodeling that underpin chronic lung disease. Future research will need to integrate biochemical markers, imaging modalities, and genetic profiles with clinical indices to develop a multidimensional risk stratification model.
Additionally, the pioneering use of the RSS in severe BPD invites further validation in diverse populations and care settings. The reproducibility of these results in different neonatal intensive care units, geographic regions, and among infants with varying comorbidities will be essential to confirm its universal applicability. Multicenter collaborative studies, alongside prospective trials testing RSS-guided extubation protocols, stand as logical next steps to consolidate this promising evidence.
From a practical perspective, the study encourages neonatal clinicians to reconsider the timing and criteria for extubation readiness. Traditionally, decisions have relied heavily on clinical stability, blood gas parameters, and subjective assessments of respiratory mechanics. The formal incorporation of RSS offers a quantifiable objective score that complements and enhances clinical judgment. This paradigm shift not only aids in decision accuracy but may also streamline multidisciplinary communication, facilitating consensus among neonatologists, respiratory therapists, and nursing staff.
Ultimately, the investigation by Zierk et al. exemplifies how precision scoring systems can bridge existing knowledge gaps in complex neonatal care challenges. The increased survival of preterm infants demands equally sophisticated approaches to manage the sequelae of prematurity like severe BPD. By harnessing tools such as the respiratory severity score, the neonatal community moves closer to a future where extubation is not a precarious gamble but a calculated, evidence-based step with predictable outcomes.
In conclusion, the identification of the respiratory severity score as a robust predictor of extubation success in infants with established grade 3 bronchopulmonary dysplasia constitutes a significant advancement in neonatal respiratory medicine. This research lays the groundwork for the development of refined extubation protocols that integrate objective respiratory metrics, potentially reducing the morbidity associated with prolonged mechanical ventilation and extubation failure. As ongoing studies build upon these findings, clinicians anticipate enhanced lung health trajectories and improved quality of life for this high-risk population. The integration of RSS-focused strategies could therefore become a cornerstone in the evolving landscape of neonatal intensive care.
Subject of Research: Association between the respiratory severity score and extubation success in severe bronchopulmonary dysplasia
Article Title: Association between the respiratory severity score and extubation success in severe bronchopulmonary dysplasia
Article References:
Zierk, A.W., Gibbs, K.A., Nelin, T.D. et al. Association between the respiratory severity score and extubation success in severe bronchopulmonary dysplasia. J Perinatol (2025). https://doi.org/10.1038/s41372-025-02396-w
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41372-025-02396-w
Tags: bronchopulmonary dysplasia managementchronic lung disease in preterm infantsextubation process in neonatesG3-BPD challengesinfant respiratory healthmechanical ventilation risksneonatal clinical outcomesneonatal intensive carepredictors of extubation successrespiratory care advancementsrespiratory severity score importanceventilator-associated complications