Detailed images of photoreceptors could advance treatment and early detection for macular degeneration and other eye diseases
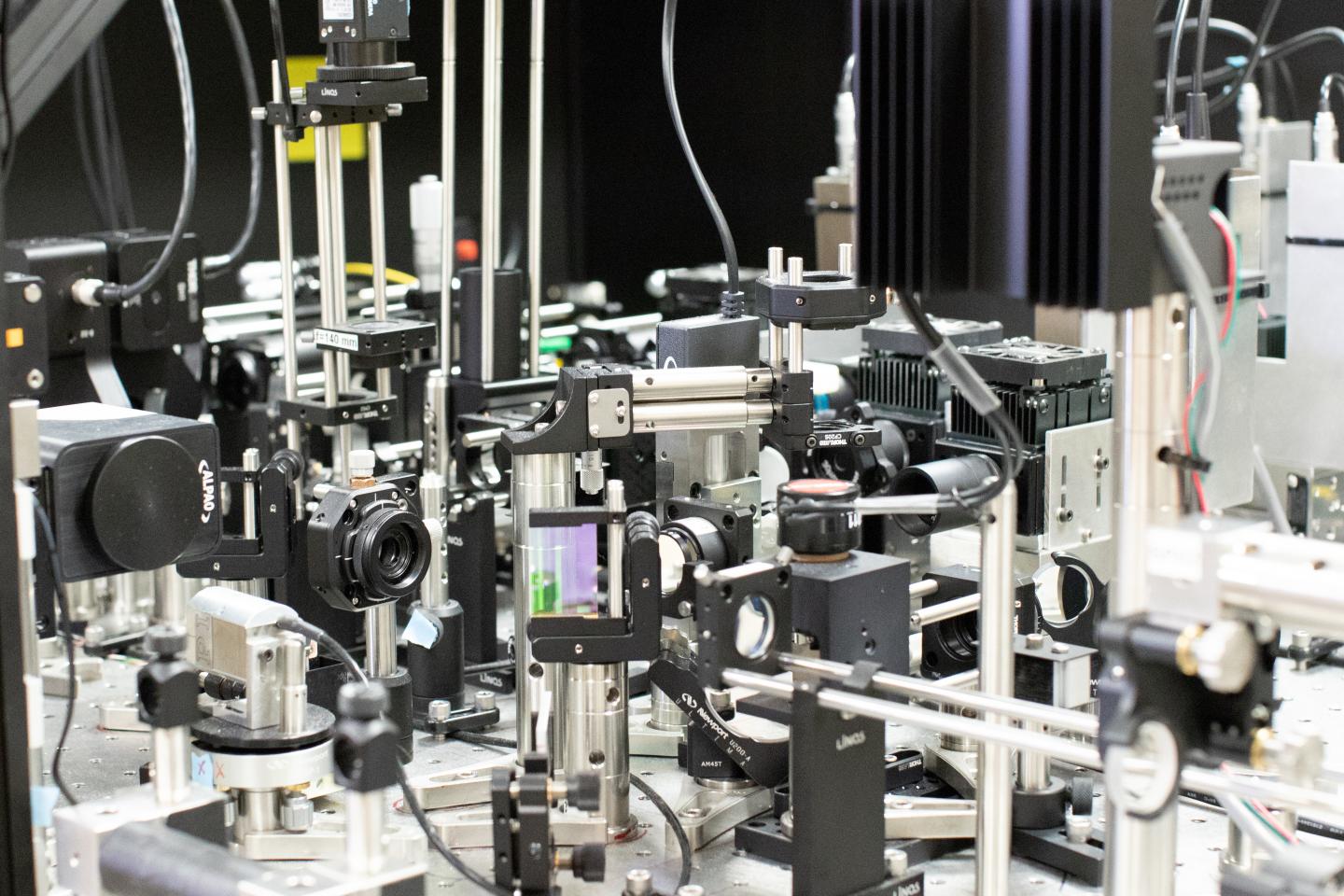
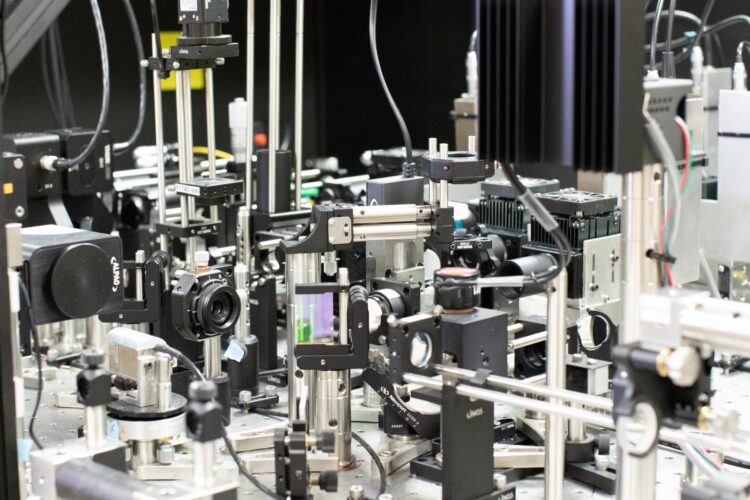
Credit: Johnny Tam, National Eye Institute
WASHINGTON — Researchers have developed a noninvasive technique that can capture images of rod and cone photoreceptors with unprecedented detail. The advance could lead to new treatments and earlier detection for retinal diseases such as macular degeneration, a leading cause of vision loss.
“We are hopeful that this technique will better reveal subtle changes in the size, shape and distribution of rod and cone photoreceptors in diseases that affect the retina,” said research team leader Johnny Tam from the National Eye Institute. “Figuring out what happens to these cells before they are lost is an important step toward developing earlier interventions to treat and prevent blindness.”
In Optica, The Optical Society’s (OSA) journal for high impact research, the researchers show that their new imaging method overcomes resolution limitations imposed by the diffraction barrier of light. The researchers accomplish this feat while using light that is safe for imaging the living human eye.
“The diffraction limit of light can now be routinely surpassed in microscopy, which has revolutionized biological research,” said Tam. “Our work represents a first step toward routine sub-diffraction imaging of cells in the human body.”
Using less light to see more
Achieving high-resolution images of photoreceptors in the back of the eye is challenging because the eye’s optical elements (such as lens and cornea) distort light in a way that can substantially reduce image resolution. The diffraction barrier of light also limits the ability of optical instruments to distinguish between two objects that are too close together. Although there are various methods for imaging beyond the diffraction limit, most of these approaches use too much light to safely image living human eyes.
To overcome these challenges, the researchers improved upon a retinal imaging technique known as adaptive optics scanning light ophthalmoscopy, which uses deformable mirrors and computational methods to correct for optical imperfections of the eye in real time.
“One might think that more light is needed to get a better image, but we demonstrate that we can improve resolution by strategically blocking light in various locations within our instrument,” said Tam. “This approach reduces the overall power of light delivered to the eye, making it ideal for live imaging applications.”
For the new approach, the researchers generated a ring-shaped, or hollow, beam of light. Using this type of beam improved the resolution across the photoreceptors but at the expense of depth resolution. To regain the lost depth resolution, the researchers used a small pinhole called a sub-Airy disk to block light coming back from the eye. They showed that this imaging approach could be used to enhance a microscopy technique called non-confocal split-detection, which is used to acquire complementary views of the photoreceptors.
Testing in the clinic
After demonstrating that imaging resolution was improved in theoretical simulations, the researchers confirmed their simulations using various test targets. They then used the new method to image rod and cone photoreceptors in five healthy volunteers at the National Institutes of Health’s Clinical Center.
The new approach yielded about a 33 percent increase in transverse resolution and 13 percent improvement in axial resolution compared to traditional adaptive optics scanning light ophthalmoscopy. Using their optimized approach, the researchers were able to see a circularly shaped subcellular structure in the center of cone photoreceptors that could not be clearly visualized previously.
“The ability to noninvasively image photoreceptors with subcellular resolution can be used to track how individual cells change over time,” said Tam. “For example, watching a cell begin to degenerate, and then possibly recover, will be an important advance for testing new treatments to prevent blindness.”
The researchers plan to image the eyes of more patients with the new technique and use the images to begin to answer fundamental questions linked to rod and cone health. For example, they are interested in visualizing rod and cone health in people who have rare genetic diseases. They say that their imaging approach could be applied to other point scanning-based microscopy and imaging approaches in which it is important to image with low levels of light.
###
The research was supported in part by NEI grants U01 EY025477 and R01 EY025231, and by the Intramural Research Program at the NEI, part of the National Institutes of Health.
Paper: R. Lu, N. Aguilera, T. Liu, J. Liu, J. P. Giannini, J. Li, A. J. Bower, A. Dubra, J. Tam, “In vivo sub-diffraction adaptive optics imaging of photoreceptors in the human eye with annular pupil illumination and sub-Airy detection,” Optica 8(3), 333-343 (2021).
DOI: https:/
About Optica
Optica is an open-access, journal dedicated to the rapid dissemination of high-impact peer-reviewed research across the entire spectrum of optics and photonics. Published monthly by The Optical Society (OSA), Optica provides a forum for pioneering research to be swiftly accessed by the international community, whether that research is theoretical or experimental, fundamental or applied. Optica maintains a distinguished editorial board of more than 60 associate editors from around the world and is overseen by Editor-in-Chief Prem Kumar, Northwestern University, USA. For more information, visit Optica.
About The Optical Society
Founded in 1916, The Optical Society (OSA) is the leading professional organization for scientists, engineers, students and business leaders who fuel discoveries, shape real-life applications and accelerate achievements in the science of light. Through world-renowned publications, meetings and membership initiatives, OSA provides quality research, inspired interactions and dedicated resources for its extensive global network of optics and photonics experts. For more information, visit osa.org.
Media Contacts:
Aaron Cohen
(301) 633-6773
[email protected]
Media Contact
James Merrick
[email protected]
Related Journal Article
http://dx.