UH researchers have identified a unique epigenetic footprint in specific types of immune cells from blood that can identify individuals with HIV that have a range of impairments in cognitive function.
Reliable biomarkers such as that identified by the researchers offer insight into how HIV-associated cognitive impairment develops but also promises improved diagnostic testing and improved treatment decisions.
The findings are published in the scientific journal Nature Scientific Reports (September 2016) by UH Mānoa scientists Lishomwa Ndhlovu, MD, PhD, and Alika Maunakea, PhD, at the John A. Burns School of Medicine (JABSOM) and collaborators at UHM and the University of California San Francisco.
“These results offer the first significant window into the mechanisms driving HIV-related brain damage and how to track the disease,” said Dr. Ndhlovu, Associate Professor in JABSOM’s Department of Tropical Medicine.
Combination antiretroviral therapies have improved HIV survival. If started early and taken daily for life, antiretroviral therapies can result in fewer non-AIDS related complications. However, HIV still impacts the brain. Around 40% of individuals even on antiretroviral therapy still suffer HIV-related neurocognitive disorders that can affect living activities.
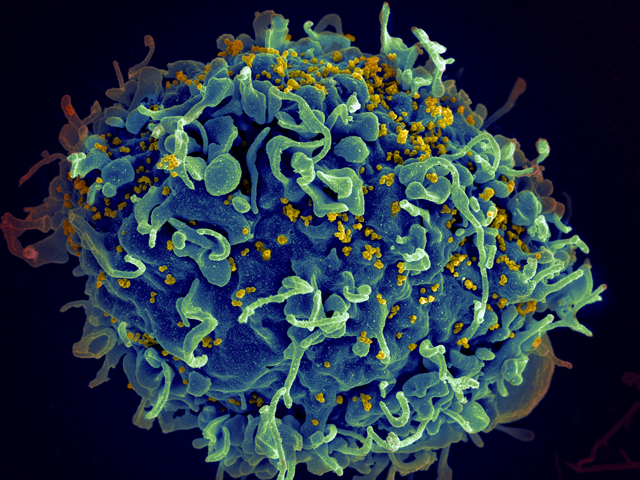
It has long been suspected that changes to cells of the monocyte/macrophage lineage, a type of immune cell, influence the development of cognitive impairment in HIV. Since HIV infection itself alters epigenetic processes in the immune system, the research team wondered whether a distinct DNA methylation profile, a major epigenetic modification where methyl groups are added to DNA, occurs in those with HIV associated-cognitive impairment and whether it exists in distinct immune cell populations from the blood.
By evaluating DNA methylation, the researchers discovered differences in gene networks and gene expression linked to the central nervous system and interactions with HIV that appeared uniquely in monocytes of HIV infected study participants with cognitive impairment.
“Strikingly, further analysis showed a strong association between DNA methylation levels of these markers in monocytes and neuropsychological test function, measured using a composite score of multiple cognitive domains,” said Dr. Maunakea, Assistant Professor, Department of Native Hawaiian Health, JABSOM and co-senior author of the study.
According to Michael Corley, PhD, a junior researcher in the Department of Native Hawaiian Health at JABSOM and lead author of the study, the field of epigenetics has ushered in a new era of discovery in immunology and neuroscience. “Combined with the advancement of DNA sequencing technologies to capture epigenetic profiles in unique clinical samples, researchers can make discoveries that were previously not possible,” said Dr. Corley.
Currently there is no treatment for individuals with HIV associated cognitive impairment. “The advancement in epigenetic therapeutics also affords promising new interventions that should be considered for the management of HIV associated cognitive impairment, provided they are selective to the appropriate immune cell target,” added Dr. Ndhlovu.
“There is still much we need to understand about how HIV affects the brain and several findings from this study are highly relevant to this field of NeuroAIDS,” said Dr. Ndhlovu.
Web Source: University of Hawaii at Manoa.
Reference List:
Glen M. Chew, Tsuyoshi Fujita, Gabriela M. Webb, Benjamin J. Burwitz, Helen L. Wu, Jason S. Reed, Katherine B. Hammond, Kiera L. Clayton, Naoto Ishii, Mohamed Abdel-Mohsen, Teri Liegler, Brooks I. Mitchell, Frederick M. Hecht, Mario Ostrowski, Cecilia M. Shikuma, Scott G. Hansen, Mark Maurer, Alan J. Korman, Steven G. Deeks, Jonah B. Sacha, Lishomwa C. Ndhlovu. TIGIT Marks Exhausted T Cells, Correlates with Disease Progression, and Serves as a Target for Immune Restoration in HIV and SIV Infection. PLOS Pathogens, 2016; 12 (1): e1005349 DOI: 10.1371/journal.ppat.1005349
The post Researchers find a potential signature of cognitive function in people living with HIV appeared first on Scienmag.





