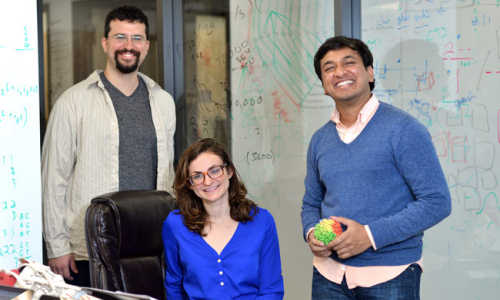
Professor of Genetics Scott Williams, PhD, of the Institute for Quantitative Biomedical Sciences (iQBS) at Dartmouth’s Geisel School of Medicine, has made two novel discoveries: first, a person can have several DNA mutations in parts of their body, with their original DNA in the rest—resulting in several different genotypes in one individual—and second, some of the same genetic mutations occur in unrelated people. We think of each person’s DNA as unique, so if an individual can have more than one genotype, this may alter our very concept of what it means to be a human, and impact how we think about using forensic or criminal DNA analysis, paternity testing, prenatal testing, or genetic screening for breast cancer risk, for example. Williams’ surprising results indicate that genetic mutations do not always happen purely at random, as scientists have previously thought. His work, done in collaboration with Professor of Genetics Jason Moore, PhD, and colleagues at Vanderbilt University, was published in PLOS Genetics journal on November 7, 2013.1
Genetic mutations can occur in the cells that are passed on from parent to child and may cause birth defects. Other genetic mutations occur after an egg is fertilized, throughout childhood or adult life, after people are exposed to sunlight, radiation, carcinogenic chemicals, viruses, or other items that can damage DNA. These later or “somatic” mutations do not affect sperm or egg cells, so they are not inherited from parents or passed down to children. Somatic mutations can cause cancer or other diseases, but do not always do so. However, if the mutated cell continues to divide, the person can develop tissue, or a part thereof, with a different DNA sequence from the rest of his or her body.
“We are in reality diverse beings in that a single person is genetically not a single entity—to be philosophical in ways I do not yet understand—what does it mean to be a person if we are variable within?” says Williams, the study’s senior author, and founding Director of the Center for Integrative Biomedical Sciences in iQBS. “What makes you a person? Is it your memory? Your genes?” He continues, “We have always thought, ‘your genome is your genome.’ The data suggest that it is not completely true.”
In the past, it was always thought that each person contains only one DNA sequence (genetic constitution). Only recently, with the computational power of advanced genetic analysis tools that examine all the genes in one individual, have scientists been able to systematically look for this somatic variation. “This study is an example of the type of biomedical research project that is made possible by bringing together interdisciplinary teams of scientists with expertise in the biological, computational and statistical sciences.” says Jason Moore, Director of the iQBS, who is also Associate Director for Bioinformatics at the Cancer Center, Third Century Professor, and Professor of Community and Family Medicine at Geisel.
Having multiple genotypes from mutations within one’s own body is somewhat analogous to chimerism, a condition in which one person has cells inside his or her body that originated from another person (i.e., following an organ or blood donation; or sometimes a mother and child—or twins—exchange DNA during pregnancy. Also, occasionally a person finds out that, prior to birth, he or she had a twin who did not survive, whose genetic material is still contained within their own body).2 Chimerism has resulted in some famous DNA cases: one in which a mother had genetic testing that “proved” that she was unrelated to two of her three biological sons.3
Williams says that, although this was a small study, “there is a lot more going on than we thought, and the results are, in some ways, astoundingly weird.”
Because somatic changes are thought to happen at random, scientists do not expect unrelated people to exhibit the same mutations. Williams and colleagues analyzed the same 10 tissue samples in two unrelated people. They found several identical mutations, and detected these repeated mutations only in kidney, liver and skeletal body tissues. Their research examined “mitochondrial DNA” (mtDNA)—a part of DNA that is only inherited from the mother.4 Technically all women would share mtDNA from one common female ancestor, but mutations have resulted in differences. The importance of Williams’ finding is that these tissue-specific, recurrent, common mutations in mtDNA among unrelated study subjects—only detected in three body tissues—are “not likely being developed and maintained through purely random processes,” according to Williams. They indicate “a completely different model …. a decidedly non-random process that results in particular mutations, but only in specific tissues.”
If our human DNA changes, or mutates, in patterns, rather than randomly; if such mutations “match” among unrelated people; or if genetic changes happen only in part of the body of one individual, what does this mean for our understanding of what it means to be human? How may it impact our medical care, cancer screening, or treatment of disease? We don’t yet know, but ongoing research may help reveal the answers.
Christopher Amos, PhD, Director of the Center for Genomic Medicine and Associate Director for Population Sciences at the Cancer Center, says, “This paper identifies mutations that develop in multiple tissues, and provides novel insights that are relevant to aging. Mutations are noticed in several tissues in common across individuals, and the aging process is the most likely contributor. The theory would be that selected mutations confer a selective advantage to mitochondria, and these accumulate as we age.” Amos, who is also a Professor of Community and Family Medicine at Geisel, says, “To confirm whether aging is to blame, we would need to study tissues from multiple individuals at different ages.” Williams concurs, saying, “Clearly these do accumulate with age, but how and why is unknown—and needs to be determined.”
As more and better data become available from high-throughput genetic analyses and high-powered computers, researchers are identifying an increasing number of medical conditions that result from somatic mutations, including neurological, hematological, and immune-related disorders. Williams and colleagues are conducting further research to examine how diseases, other than cancer or even benign conditions, may result from somatic changes.5 Williams, Moore and Amos will employ iQBS’s Discovery supercomputer for next-generation sequencing to process subjects’ DNA data.6 Future analyses will include large, whole-genome sequencing of the data for the two individuals studied in the current report.
Williams explains, “We know that cancer is caused by mutations that cause a tumor. But in this work, we chose to study mutations in people without any cancer. Knowing how we accumulate mutations may make it easier to separate genetic signals that may cause cancer from those that accumulate normally without affecting disease. It may also allow us to see that many changes that we thought caused cancer do not in many situations, if we find the same mutations in normal tissues.”
Just as our bodies’ immune systems have evolved to fight disease, interestingly, they can also stave off the effects of some genetic mutations. Williams states that, “Most genetic changes don’t cause disease, and if they did, we’d be in big trouble. Fortunately, it appears our systems filter a lot of that out.”
Mark Israel, MD, Director of Norris Cotton Cancer Center and Professor of Pediatrics and Genetics at Geisel, says, “The fact that somatic mutation occurs in mitochondrial DNA apparently non-randomly provides a new working hypothesis for the rest of the genome. If this non-randomness is general, it may affect cancer risks in ways we could not have previously predicted. This can have real impact in understanding and changing disease susceptibility.”
Story Source:
The above story is based on materials provided by The Geisel School of Medicine at Dartmouth.