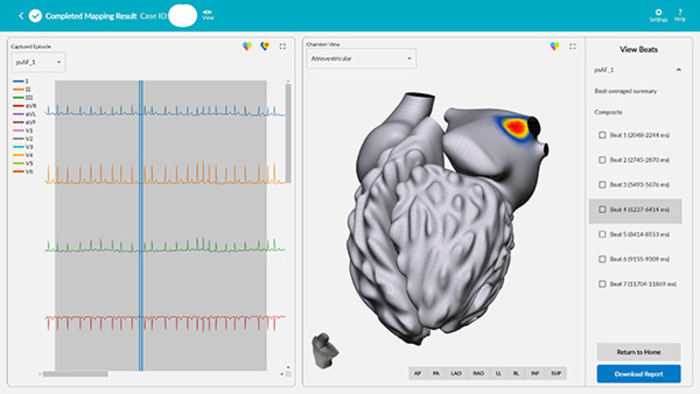
A new way of treating arrhythmias, including atrial fibrillation (AF) — the most common heart arrhythmia diagnosis in clinical practice — has debuted at UC San Diego Health. vMap is a non-invasive, computational mapping system that produces a three-dimensional, interactive map of arrhythmia hotspots anywhere in the heart, including all four chambers of the organ, the septal wall and the outflow tracts. The system, which maps in a matter of minutes, requires only the data from a standard 12-lead electrocardiogram (ECG) to work.
Credit: Vektor Medical
A new way of treating arrhythmias, including atrial fibrillation (AF) — the most common heart arrhythmia diagnosis in clinical practice — has debuted at UC San Diego Health. vMap is a non-invasive, computational mapping system that produces a three-dimensional, interactive map of arrhythmia hotspots anywhere in the heart, including all four chambers of the organ, the septal wall and the outflow tracts. The system, which maps in a matter of minutes, requires only the data from a standard 12-lead electrocardiogram (ECG) to work.
AF is an irregular and often rapid heart rhythm that can cause stroke and heart failure. It affects more than six million Americans, resulting in more than 41,000 deaths annually. The standard of care for treating the condition is ablation, in which small, steerable catheters are inserted into the heart to burn or freeze specific areas responsible for the electrical signals causing the abnormal heartbeat.
But how are those specific areas located? Traditional arrhythmia-mapping techniques are labor-and time-intensive, and physicians are only able to achieve complete success in a limited number of ablation procedures due to the lack of information about arrhythmia source locations. AF recurs following catheter ablation in 20 to 40 percent of cases, according to the Journal of Atrial Fibrillation.
Existing invasive mapping has limitations in speed, efficacy and safety, and existing non-invasive mapping requires additional steps, such as magnetic resonance imaging and computerized tomography, and cannot map the entire heart organ. To shorten procedure times and improve ablation success, electrophysiologists need to be able to visualize arrhythmia hotspots in the heart quickly and accurately.
“My team and I experienced first-hand the limitations of the current standard of care for understanding and treating arrhythmias.” said David Krummen, MD, cardiac electrophysiologist at UC San Diego Health and professor of medicine at University of California San Diego School of Medicine, who co-invented vMap and serves as clinical advisor to Vektor Medical, its manufacturer.
“We designed vMap to improve ablation outcomes by rapidly providing arrhythmia source information to the physician. We want this technology to increase first-pass ablation success, decrease procedural risk, and improve the care of patients with heart rhythm abnormalities.”
vMap — which received Food and Drug Administration clearance in November 2021 — converts ECG data into 2D and 3D arrhythmia source maps using data leveraged from millions of arrhythmia simulations performed by technology resources, including the UC San Diego’s San Diego Supercomputer Center. The results from vMap’s first clinical study will be published later this year.
vMap is now available to assist physicians and electrophysiologists at UC San Diego Health with arrhythmia analysis and mapping. To learn more about vMap, please speak to your physician.
# # #



