In a groundbreaking study recently published in npj Parkinson’s Disease, researchers led by Fox, S.H., Luca, D.G., and Postuma, R.B. have revisited the 2015 Movement Disorder Society (MDS) diagnostic criteria for Parkinson disease (PD). This comprehensive reassessment leverages the invaluable insights derived from autopsy-confirmed cases, providing an unprecedented opportunity to refine diagnostic accuracy in a condition notorious for its clinical complexity and heterogeneity. With Parkinson disease being one of the most prevalent neurodegenerative disorders worldwide, affecting millions of individuals, the implications of this study extend far beyond academic discourse into the realm of clinical practice and patient care.
The original 2015 MDS diagnostic criteria marked a significant advancement in standardizing PD diagnosis, incorporating clinical features such as bradykinesia, rigidity, and resting tremor, along with supportive and exclusionary criteria. Yet, despite these frameworks, diagnostic accuracy in living patients remains suboptimal, often leading to delayed or incorrect diagnoses. Given that Parkinson disease encompasses diverse pathophysiological mechanisms and overlapping syndromes, the integration of neuropathological verification from autopsy cases offers an invaluable gold standard against which clinical criteria can be rigorously tested and refined.
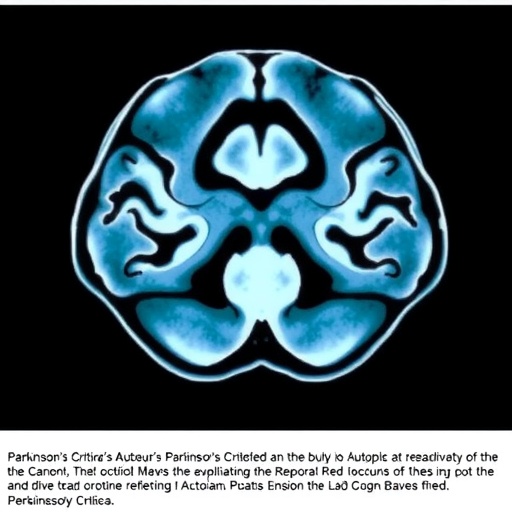
Autopsy-confirmed cases serve as the ultimate reference for validating clinical diagnoses post mortem by revealing the definitive distribution and extent of alpha-synuclein pathology characteristic of PD. The study’s approach involved a meticulous review of clinical records alongside comprehensive neuropathological examinations, encompassing both typical Lewy body disease manifestations and atypical presentations. This dual review challenges prior assumptions embedded in the diagnostic algorithm and questions the sensitivity and specificity of the 2015 criteria when confronted with complex and mixed pathologies that either mimic or coexist with PD.
One of the pivotal revelations from this work is the identification of critical nuances in the presentation of motor and non-motor symptoms that were underappreciated in the older criteria. For instance, certain early non-motor indicators such as hyposmia, REM sleep behavior disorder, and subtle autonomic dysfunction appeared to be more predictive of autopsy-confirmed PD than previously thought. These findings underscore the necessity of integrating a broader symptom complex into diagnostic formulations to improve early and differential diagnosis, especially since non-motor symptoms often precede motor manifestations by years.
Moreover, the study reevaluates the role of exclusion criteria that were originally incorporated to rule out alternative diagnoses such as multiple system atrophy (MSA) or progressive supranuclear palsy (PSP). The autopsy data revealed overlapping neuropathological features in some cases previously dismissed under clinical criteria, suggesting that the dichotomization between PD and these atypical parkinsonian disorders may be more porous than recognized. This calls for a paradigm shift toward a more nuanced, perhaps spectrum-based understanding of parkinsonian disorders.
Neuroimaging and biomarker data, which have gained prominence since the 2015 guidelines, were also retrospectively assessed in conjunction with autopsy findings. The study emphasizes that while currently available imaging techniques such as DaTSCAN or MRI provide supportive information, their diagnostic specificity remains insufficient in isolation. The absence of definitive biological markers continues to be a major hurdle in PD diagnosis, cementing the importance of pathological confirmation in refining clinical criteria.
Insights into genetic factors emerged from the cohort analysis as well, revealing that certain genetic mutations traditionally associated with atypical parkinsonism may manifest clinically resembling idiopathic PD. This genetic heterogeneity further complicates the clinical picture and highlights the potential for genetics-informed diagnostic criteria that could one day complement or enhance clinical assessments.
The implications for clinical trials are profound. Misdiagnosis or delayed diagnosis can dilute the impact of therapeutic interventions, as trial populations may inadvertently include individuals without true PD pathology. The updated criteria informed by this autopsy study pave the way for more accurate participant selection, thereby enhancing the validity and efficacy of future therapeutic developments.
Beyond refining diagnosis, the research promotes a multidimensional approach to patient evaluation, advocating for detailed longitudinal phenotyping encompassing motor, cognitive, psychiatric, and autonomic domains. Such granularity is not only essential for clinical precision but also for tailoring personalized treatment plans, given the wide variation in disease progression and symptomatology.
The study’s authors also discuss the potential for artificial intelligence and machine learning to assimilate complex clinical, imaging, and genetic data to aid in diagnosis. However, these technologies still require anchoring to validated pathological benchmarks, reinforcing the continued relevance of autopsy studies in the era of digital medicine.
A notable challenge highlighted is the limited availability of autopsy-confirmed data, which underscores the need for expanded brain donation programs and international collaborative efforts to build robust neuropathological databases. Such initiatives are vital for perpetually refining diagnostic frameworks in neurodegenerative diseases.
In conclusion, this landmark study represents a crucial recalibration of the diagnostic landscape for Parkinson disease. By confronting clinical criteria with neuropathological realities, Fox, Luca, Postuma, and their colleagues have illuminated pathways toward more accurate, earlier, and personalized diagnosis. This progress promises to transform both research methodologies and clinical paradigms, ultimately enhancing patient outcomes in a disease that continues to exact a heavy toll on global health.
The ongoing evolution of diagnostic criteria exemplifies the dynamic interplay between clinical observation and pathological truth, a synergy indispensable for conquering the complexities of Parkinson disease. Future research expanding on these findings will undoubtedly explore novel biomarkers, advanced neuroimaging modalities, and integrative computational approaches informed by this foundational work. This deepened understanding fuels hope for breakthrough therapies and improved quality of life for millions affected by Parkinson disease worldwide.
Subject of Research: Reassessment and refinement of the 2015 MDS diagnostic criteria for Parkinson disease through analysis of autopsy-confirmed cases.
Article Title: Revisiting the 2015 MDS diagnostic criteria for Parkinson disease: insights from autopsy-confirmed cases.
Article References:
Fox, S.H., Luca, D.G., Postuma, R.B. et al. Revisiting the 2015 MDS diagnostic criteria for Parkinson disease: insights from autopsy-confirmed cases. npj Parkinsons Dis. (2025). https://doi.org/10.1038/s41531-025-01206-6
Image Credits: AI Generated
Tags: 2015 MDS criteria reevaluationalpha-synuclein distribution analysisautopsy-confirmed Parkinson casesbradykinesia and rigidity assessmentclinical accuracy in Parkinson diagnosisclinical practice in neurodegenerationimplications for patient care in PDmovement disorders society guidelinesneurodegenerative disorders researchParkinson disease diagnostic criteriaParkinson disease pathophysiologyrefining Parkinson disease diagnosis