In a groundbreaking new study published in Diabetes Therapy, researchers have investigated the efficacy of Polyethylene Glycol Loxenatide when used in conjunction with basal insulin. This innovative therapeutic combination aims to enhance glycemic control in patients suffering from type 2 diabetes mellitus (T2DM), a condition affecting millions globally. The growing incidence of T2DM has put significant pressure on healthcare systems, creating an urgent need for effective treatment options. The interplay between drug administration and patient outcomes is crucial, and the latest findings present promising implications for clinical practice.
The study was conducted by a team led by Liu, Zhang, and Zhao, who have meticulously evaluated real-world evidence from a diverse population of T2DM patients. Utilizing a retrospective design, the researchers analyzed data to discern trends and outcomes associated with Polyethylene Glycol Loxenatide therapy combined with basal insulin. This combination treatment offers a potentially valuable strategy for optimizing diabetes management. The authors emphasize the importance of real-world studies, as they provide insights that may not be readily observable in randomized clinical trials.
Polyethylene Glycol Loxenatide belongs to the class of GLP-1 receptor agonists, known for promoting insulin secretion while simultaneously inhibiting glucagon release. Its unique formulation allows for sustained release, improving patient compliance and overall metabolic outcomes. Combining this agent with basal insulin offers a dual approach to managing blood sugar levels, mitigating the need for higher doses of insulin, which can lead to adverse effects such as weight gain and hypoglycemia.
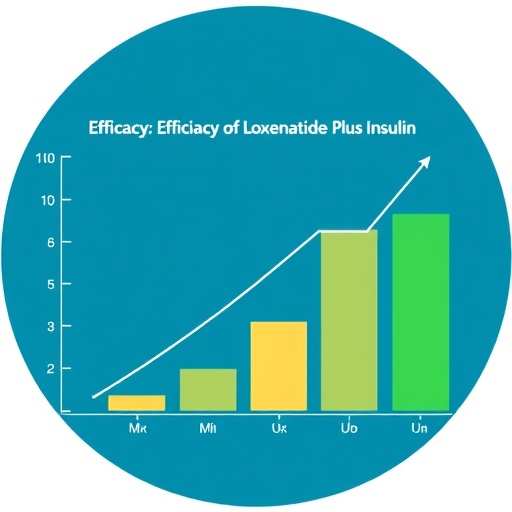
One of the critical findings of the study is the observable improvement in glycemic control among patients who adhered to the combination therapy. Blood glucose levels were significantly lowered, demonstrating a superior response compared to those treated with basal insulin alone. The researchers highlighted that the continuing rise in glycemic levels can lead to long-term complications, including cardiovascular issues and neuropathy, thus underscoring the need for effective management strategies.
Another essential aspect of the research delved into patient adherence rates. With the growing complexity of diabetes management regimens, treatment adherence remains a major obstacle to effective control. The dual-action mechanism of Polyethylene Glycol Loxenatide appears to enhance the overall satisfaction of patients regarding their diabetes treatment, potentially leading to improved adherence rates. This finding could have far-reaching implications for healthcare providers aiming to tailor treatments to individual patient needs.
Safety profiles of medication combinations are also a focal point of this research. By extending the investigation into adverse effects, the authors demonstrated that combining Polyethylene Glycol Loxenatide with basal insulin did not lead to increased incidences of hypoglycemia when compared to traditional insulin regimens alone. Furthermore, the study reported no significant uptick in gastrointestinal side effects commonly associated with GLP-1 receptor agonists, further adding to the therapeutic allure of this combination.
As the researchers analyzed patient-reported outcomes, the quality of life measurements solidified their findings. Those engaged in the combination therapy noted a marked improvement in daily functioning, which is critical in managing a chronic condition like diabetes. Patients reported increased energy levels and decreased anxiety regarding fluctuating blood sugar levels, presenting a more holistic perspective on diabetes management.
The implications of this study extend beyond merely improving glucose control. The research highlights how innovative treatment combinations can fit into modern lifestyle adjustments. For diabetes patients navigating work-life balance, an effective therapeutic regimen enables them to prioritize their health without dictating their daily activities. The significance of such findings cannot be overlooked as healthcare practitioners and patients alike seek manageable solutions.
For healthcare practitioners, the insights derived from this research emphasize the importance of personalized treatment plans. By understanding the specific needs and responses of patients, clinicians can effectively tailor regimens that harness the benefits of both Polyethylene Glycol Loxenatide and basal insulin. This study encourages ongoing dialogue in the medical community about optimizing diabetes treatment and decision-making.
As advances continue in the diabetes pharmaceutical landscape, this research serves as a catalyst for further inquiry into combination therapies. With numerous clinical trials already underway investigating other SGLT-2 inhibitors and various GLP-1 receptor agonists, it stands to reason that healthcare providers must stay abreast of emerging evidence. These evolving treatment paradigms will undoubtedly reshape the future of diabetes management.
Moreover, the higher efficacy reported in this study could have positive ramifications for cost-effectiveness analyses, as better-managed diabetes is associated with reduced long-term healthcare costs. Policy-makers and health insurance providers may find themselves reassessing coverage strategies in light of new evidence that signifies more effective diabetes management pathways.
The authors also posited that future studies should focus on longer-term follow-ups to assess the sustainability of the glycemic control achieved with this combination therapy. Established benchmarks for diabetes health outcomes could guide ongoing evaluations, ultimately leading to refined clinical guidelines. The healthcare community is eager for tangible results to guide succinct therapeutic recommendations.
In conclusion, the findings surrounding the efficacy of Polyethylene Glycol Loxenatide alongside basal insulin represent a significant advancement in diabetes care. The combination therapy not only showcases enhanced glycemic control but also addresses patient adherence and overall well-being. As part of the dialogue surrounding innovative diabetes treatments, this study potentially paves the way for improved clinical outcomes and quality of life for millions grappling with this challenging disease.
In a rapidly evolving medical landscape, continuous exploration and refinement of treatment modalities will be key to addressing the complex needs of T2DM patients. As researchers build on this knowledge, the diabetes community can look forward to more nuanced and effective strategies aimed at achieving optimal metabolic health.
Subject of Research: Efficacy of Polyethylene Glycol Loxenatide in Combination with Basal Insulin in Patients with Type 2 Diabetes Mellitus
Article Title: Efficacy of Polyethylene Glycol Loxenatide in Combination with Basal Insulin in Patients with Type 2 Diabetes Mellitus: A Retrospective Real-World Study
Article References: Liu, X., Zhang, Y., Zhao, Ll. et al. Efficacy of Polyethylene Glycol Loxenatide in Combination with Basal Insulin in Patients with Type 2 Diabetes Mellitus: A Retrospective Real-World Study. Diabetes Ther 16, 1581–1592 (2025). https://doi.org/10.1007/s13300-025-01737-4
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s13300-025-01737-4
Keywords: Type 2 Diabetes Mellitus, Polyethylene Glycol Loxenatide, Basal Insulin, Glycemic Control, Combination Therapy.
Tags: clinical implications of diabetes therapiescombination therapy for diabetes managementefficacy of Loxenatide and insulinGLP-1 receptor agonists in diabetesglycemic control in type 2 diabeteshealthcare challenges in managing diabetes mellitusimproving patient compliance in diabetesinnovative treatments for type 2 diabetesinsulin and GLP-1 receptor agonist synergyPolyethylene Glycol Loxenatide for T2DMreal-world study on diabetes treatmentretrospective analysis of diabetes outcomes