Deep Brain Stimulation (DBS) has revolutionized the treatment landscape for Parkinson’s disease, offering relief when medications no longer provide adequate symptom control. Yet, the intricacies of DBS surgery demand precision that often hinges on real-time electrophysiological feedback to guide electrode placement. In a pioneering study soon to be published in npj Parkinson’s Disease, researchers led by Issabekov, Al-Fatly, and Mousavi delve into the nuanced role of the anesthetic propofol during DBS, revealing a graded influence on electrophysiology-guided navigation that could reshape surgical protocols.
Traditionally, DBS surgery involves awake patients to capture reliable electrophysiological signals from deep brain structures such as the subthalamic nucleus (STN). These signals inform surgeons about the ideal trajectory and final placement of stimulation electrodes, directly impacting clinical outcomes. However, keeping patients awake presents challenges including discomfort, anxiety, and movement, prompting interest in anesthetic strategies that do not compromise intraoperative neurophysiological data. Propofol, a commonly used anesthetic agent for sedation, has been considered in this context, but its effects on neuronal recordings remained inadequately characterized—until now.
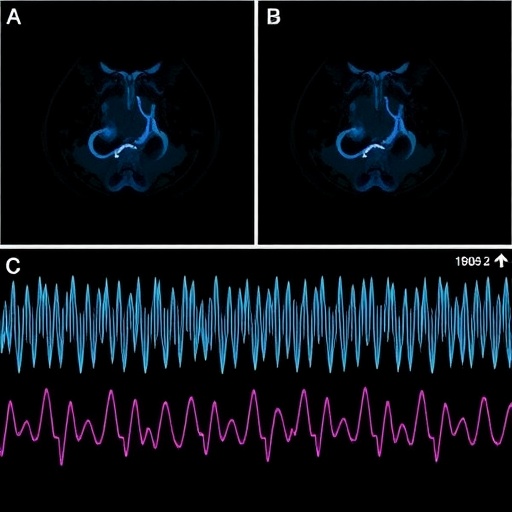
The study meticulously explores how varying doses of propofol impact the electrophysiological signatures recorded during DBS procedures. Employing sophisticated neurophysiological mapping combined with computational analytics, the team quantified changes in neural firing rates, signal-to-noise ratios, and oscillatory patterns across different propofol infusion levels. Their work elucidates a dose-dependent modulation of neuronal activity where low-dose propofol preserves critical electrophysiological features, whereas higher doses progressively dampen signal clarity and reduce the discriminatory power needed for precise electrode targeting.
This breakthrough insight addresses a crucial tradeoff in DBS surgeries: balancing patient comfort through sedation against the preservation of high-fidelity electrophysiological guidance. The graded effect of propofol implies that surgeons can strategically titrate sedation to optimize both dimensions, potentially expanding the use of asleep DBS surgeries without sacrificing outcome efficacy. Such calibration can herald a new era where patients benefit from more tolerable surgical experiences combined with the neuroscience rigor required for therapeutic success.
Importantly, the study offers a refined computational framework to evaluate electrophysiological changes in real time, enabling immediate feedback during surgery. This system analyses multiunit neural activity and local field potentials with enhanced sensitivity, flagging deviations indicative of excessive anesthetic interference. By integrating this technology, surgical teams can dynamically adjust propofol levels, harnessing a fine balance between sedation and neurophysiological monitoring.
One of the striking revelations from this research is how specific neuronal firing patterns, previously deemed reliable biomarkers for target localization, show differential susceptibility to anesthesia. The beta oscillations typically recorded in the STN, linked closely to Parkinsonian motor symptoms, exhibited attenuation at moderate propofol doses. This attenuation blurs the electrophysiological signature that surgeons rely on, underscoring the critical need for targeted anesthetic dosing.
Beyond the immediate clinical implications, the findings also provoke a deeper understanding of how anesthetics modulate basal ganglia circuits at a cellular level. Propofol’s effects extend beyond mere sedation to influencing synaptic activity and network synchrony, with consequences observable through the electrophysiology-guided approach described. This dual perspective enriches our grasp of neuropharmacology as well as neurosurgical strategy.
The authors emphasize that their results do not advocate for the abandonment of awake DBS altogether, but instead call for a refined, patient-specific approach. Certain patients might withstand low-dose propofol sedation without compromising mapping fidelity, improving their surgical experience and reducing intraoperative stress. Conversely, the approach allows identification of scenarios where awake monitoring remains indispensable.
Methodological rigor marks this investigation, as it draws on a sizable patient cohort undergoing subthalamic DBS with multimodal electrophysiological recordings. Advanced machine learning algorithms decoded neural signals under varying anesthetic conditions, adding robustness to the conclusions and setting a new standard for bridging anesthetic pharmacodynamics with neurosurgical precision.
Critically, these advancements may help mitigate some of the current barriers to more widespread adoption of DBS. Patient reluctance and the challenge of tolerating awake surgery often deter timely intervention. Tailoring propofol administration with electrophysiological feedback promises a gentler pathway to surgical candidacy, reducing psychological burdens and enabling intervention at earlier disease stages.
Integrating these findings into clinical practice will likely necessitate updates to DBS protocols and training, equipping surgical teams with both the pharmacological understanding and neurophysiological interpretative skills required. Protocols for intraoperative sedation must carefully define propofol titration schemes that ensure signal integrity while prioritizing patient safety and comfort.
This novel research also beckons further investigation into other anesthetic agents and combinations, assessing their differential impacts on electrophysiological guidance. Comparative studies could delineate an optimal anesthesia cocktail tailored not only to procedural needs but also to individual patient neurophysiology and pathology.
Moreover, the potential application of this graded anesthetic approach might extend beyond Parkinson’s disease to other movement disorders and neuropsychiatric conditions amenable to DBS, amplifying its clinical significance. Comprehensive electrophysiological monitoring under sedation could become a universal paradigm in functional neurosurgery.
In conclusion, the work spearheaded by Issabekov, Al-Fatly, Mousavi, and colleagues signals a paradigm shift in DBS surgery. Their comprehensive characterization of propofol’s graded effects introduces a new layer of sophistication into surgical navigation, blending neuropharmacology, computational neuroscience, and clinical neurology. As this knowledge disseminates and protocols evolve, we stand poised to make DBS procedures simultaneously more patient-friendly and neurophysiologically precise, a triumphant step toward smarter and gentler neuromodulation therapies.
The dawn of precision anesthesia in functional neurosurgery shines brightly, fueled by this groundbreaking evidence that anesthetic dosing can be finely tuned to preserve the brain’s electrophysiological dialogue—an advance that may transform millions of lives burdened by Parkinson’s disease worldwide.
Subject of Research:
The graded effect of propofol on electrophysiology-guided navigation during deep brain stimulation (DBS) surgery for Parkinson’s disease.
Article Title:
The graded effect of propofol in electrophysiology-guided navigation during deep brain stimulation surgery.
Article References:
Issabekov, G., Al-Fatly, B., Mousavi, M. et al. The graded effect of propofol in electrophysiology-guided navigation during deep brain stimulation surgery. npj Parkinsons Dis. (2026). https://doi.org/10.1038/s41531-025-01243-1
Image Credits: AI Generated
Tags: anesthetic strategies in neurosurgeryDBS clinical outcomesDeep Brain Stimulation surgeryelectrophysiology-guided navigationintraoperative neurophysiological dataneural firing rate changesParkinson’s disease treatmentpatient comfort during DBSpropofol anesthetic effectssedation strategies in DBSsubthalamic nucleus recordingssurgical electrode placement precision