In the evolving landscape of neonatal care and neurodevelopmental prognosis, a groundbreaking study has emerged that may recalibrate how clinicians forecast outcomes in preterm infants. Published in the Journal of Perinatology, the research conducted by Ancora, Tarocco, Natile, and colleagues scrutinizes two pivotal neurological assessment tools: amplitude-integrated electroencephalography (aEEG) at 32 weeks postmenstrual age versus magnetic resonance imaging (MRI) performed at term equivalent age. This study delves deeply into the comparative predictive power of these modalities, offering fresh insights into early neurodevelopmental diagnostics.
Preterm birth, inherently linked to a plethora of neurodevelopmental challenges, necessitates precise, early prediction methods to optimize interventions and long-term care strategies. Historically, neonatologists have relied heavily on MRI near term to delineate structural brain abnormalities and forecast developmental trajectories. However, this protocol is resource-intensive and often delayed in pinpointing infants at risk for subtle neurological impairments. Enter aEEG—a bedside, continuous neurophysiological monitoring technique offering real-time cerebral activity data much earlier in development at around 32 weeks gestational age.
The investigative team set out to rigorously evaluate whether aEEG at this early time point could rival, or even surpass, the predictive accuracy of MRI conducted weeks later. By systematically analyzing longitudinal neurodevelopmental follow-up data at two years corrected age, the researchers established correlations between initial aEEG patterns, MRI findings, and eventual cognitive, motor, and behavioral outcomes. These insights bear profound implications for neonatal intensive care unit (NICU) protocols and parental counseling frameworks.
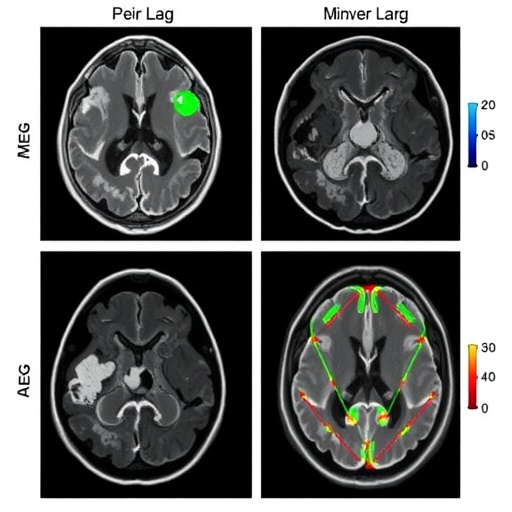
aEEG, as a simplified derivative of conventional EEG, captures cerebral electrical activity through limited channel recordings, enabling detection of background patterns indicative of maturational status or pathologic deviations such as discontinuity or burst suppression. In preterm infants, the maturation of these patterns reflects synaptic and neuronal network development, thereby serving as a potential biomarker for future neurodevelopmental trajectories. The study meticulously scored aEEG traces per standardized criteria, emphasizing continuity, sleep-wake cycling presence, and pathological features.
Conversely, MRI at term equivalent age provides high-resolution structural images revealing white matter injuries, ventriculomegaly, and cortical and subcortical abnormalities. Although comprehensive, MRI assessments are snapshots subject to interpretation variability and may miss transient functional dysfunctions detectable by electrophysiological means. This study underscores the complementary nature of functional assessments like aEEG juxtaposed with anatomical MRI, fostering a more nuanced prognostic model.
Analyzing a robust cohort of preterm neonates, ranging between 28 and 32 weeks gestational age at enrollment, the researchers employed advanced statistical modeling to reconcile early functional biomarkers with later structural anomalies and developmental milestones. Intriguingly, aEEG abnormalities detected at 32 weeks consistently correlated with adverse neurodevelopmental outcomes, including cognitive delays and motor impairments, sometimes even outperforming MRI markers in predictive fidelity.
Importantly, the study highlights the temporal advantage of aEEG, allowing clinicians to identify infants at risk weeks before term equivalent MRI is feasible. This early warning capability paves the path for implementing neuroprotective strategies, such as targeted physiotherapy, environmental modifications, and pharmacologic interventions, aimed at mitigating the trajectory towards severe disability. The capacity for bedside application enhances feasibility in diverse clinical settings, including resource-constrained environments.
The researchers also addressed the limitations inherent to both modalities. aEEG’s sensitivity to artifact and operator dependency necessitate rigorous training and protocol standardization to maximize reliability. Likewise, MRI’s lack of functional assessment means certain neurological risks may be underestimated if structural changes are subtle or absent. By integrating aEEG findings with MRI data, a more holistic neurodevelopmental risk profile emerges, empowering caregivers with actionable intelligence.
Additionally, this research underscores significant interdisciplinary collaboration, involving neonatologists, neurophysiologists, radiologists, and developmental pediatricians, emphasizing the critical need for cohesive evaluation frameworks in neonatal neurology. This synergy enhances not only diagnostic precision but also fosters longitudinal monitoring that adapts to evolving neurodevelopmental presentations in preterm survivors.
This study’s implications transcend immediate clinical utility, potentially influencing policy directives and standard-of-care guidelines to incorporate early aEEG screening as a routine component of preterm infant assessment. The cost-effectiveness of aEEG, combined with its prognostic potency, suggests that widespread adoption could democratize early detection efforts globally, thus improving neurodevelopmental outcomes on a public health scale.
Furthermore, these findings stimulate avenues for future research aimed at refining aEEG algorithms through machine learning methodologies, enhancing pattern recognition, and personalized outcome predictions. Integration of multimodal data streams — combining electrophysiological, imaging, and genetic information — could revolutionize neonatal neurology, steering it towards precision medicine paradigms.
While challenges remain, including establishing universal normative aEEG data across diverse populations and standardizing MRI interpretation criteria, the current evidence positions aEEG at 32 weeks as a formidable tool in the neurodevelopmental prognostication arsenal. It redefines temporal boundaries in assessing preterm brain health, offering hope for earlier intervention and improved quality of life for these vulnerable infants.
In a field historically constrained by delayed diagnostic indicators, this research marks a paradigm shift, elevating functional cerebral monitoring to the forefront of neonatal care. Ancora and colleagues’ work exemplifies how bridging electrophysiological and imaging realms can yield richer insights into the enigmatic development of the premature brain.
Ultimately, this seminal study illuminates the path forward, where technological innovation and clinical acumen converge to transform outcomes for preterm infants worldwide. As neonatal care continues to evolve, embracing dynamic, early-assessment strategies like aEEG heralds a new era in safeguarding the neurodevelopmental futures of our smallest patients.
Subject of Research: Neurodevelopmental prediction in preterm infants using early amplitude-integrated electroencephalography versus term MRI
Article Title: Neurodevelopmental forecasting in preterms: aEEG at 32 weeks vs. MRI at term in predicting 2-year outcomes
Article References:
Ancora, G., Tarocco, A., Natile, M. et al. Neurodevelopmental forecasting in preterms: aEEG at 32 weeks vs. MRI at term in predicting 2-year outcomes. J Perinatol (2025). https://doi.org/10.1038/s41372-025-02452-5
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41372-025-02452-5
Tags: aEEG vs MRI comparisonamplitude-integrated electroencephalographyearly prediction methods for preterm infantslongitudinal follow-up in neonatal caremagnetic resonance imaging in neonatologyneonatal neurodevelopmental assessmentneurodevelopmental prognosis in preterm birthoptimizing interventions for preterm infantspredicting subtle neurological impairmentspreterm infant outcomesreal-time monitoring of cerebral activityresource-intensive neonatal diagnostics