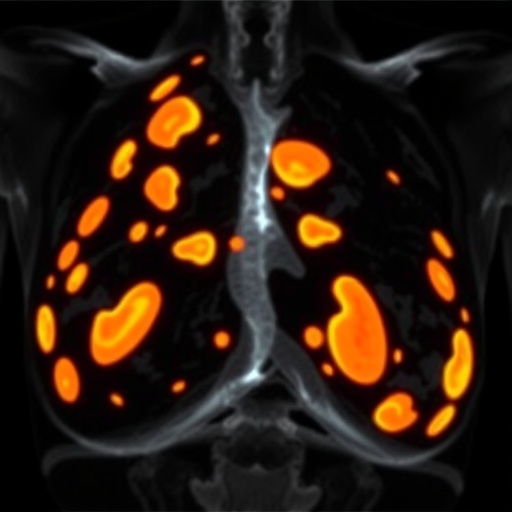
In a groundbreaking effort to combat breast cancer, researchers have introduced an innovative model that integrates microcalcifications with patient risk factors to enhance early detection. Breast cancer remains one of the most prevalent forms of cancer among women worldwide, and early intervention is paramount to improving survival rates. The traditional methods of diagnosing breast cancer often rely solely on imaging technologies, such as mammograms, which may overlook critical risk indicators that can signal an impending health crisis. The model proposed by Sreelekshmi, Pavithran, and Nair aims to bridge this gap, offering a more comprehensive approach to breast cancer prediction.
Microcalcifications are small deposits of calcium that appear as tiny white spots on mammograms. Their presence can indicate the potential for breast cancer, but they do not always result in a positive diagnosis. By developing an integrated model that takes into account individual patient risk factors, the research team aims to refine the predictive accuracy of microcalcifications. This duo of indicators—microcalcifications and personalized risk assessments—creates a robust foundation for predicting breast cancer at an earlier stage than previously possible.
The significance of using a patient-centered approach cannot be overstated. Each woman’s risk factors are uniquely defined by genetic predispositions, family history of breast cancer, lifestyle choices, and other health conditions. Traditional diagnostic methods often fail to adequately account for these varied influences, leading to missed opportunities for timely intervention. The researchers hypothesize that by creating a tailored model, clinicians can more effectively identify high-risk patients who may benefit from proactive monitoring and early detection strategies.
In their study, the authors utilized an extensive dataset that included a wide array of clinical information, imaging results, and patient demographics. The model’s algorithms dynamically process this data, allowing for real-time analysis as new patient information becomes available. The integration of machine learning techniques enhances the model’s ability to learn from emerging trends and patterns, which encourages continuous improvement in predictive capability.
One striking feature of the integrated model is its ability to continuously evolve, adapting to new findings and correlations as they emerge in the ongoing fight against breast cancer. By harnessing the latest advancements in artificial intelligence, the model remains at the forefront of predictive analytics in medicine. This state-of-the-art approach is a testament to the potential of AI in transforming healthcare, making it not only a tool for diagnosis but also a partner in preventative care.
The predictive model’s impact is expected to be multifaceted. First, it holds the potential to significantly reduce false positives in mammography screenings, which can lead to unnecessary biopsies and anxiety for patients. Reducing these instances could alleviate some of the emotional and financial burdens that many women face when navigating breast cancer screenings. Furthermore, by accurately identifying those at risk, healthcare providers can focus resources on individuals who truly need them, enhancing the efficiency of breast cancer screening programs.
As the model continues to be tested in clinical environments, the potential for widespread implementation raises questions about healthcare accessibility and equity. It is crucial for practitioners to ensure that this level of advanced screening is available to diverse populations, particularly those who may be at higher risk but lack access to cutting-edge medical technologies. Addressing disparities in healthcare will be a key consideration as researchers and providers look to deploy this model broadly.
What sets this research apart is not just its technical advancements but also its alignment with the growing movement towards personalized medicine. The understanding that no two patients are alike underlines the importance of tailored healthcare solutions. As the field of oncology progresses, the shift from one-size-fits-all to precision medicine remains a critical focal point. By placing individual risk factors at the helm of cancer predictions, the integrated model underscores a pivotal trend towards individualization in treatment and diagnostic strategies.
Looking forward, the innovation presents an avenue for further research and development. Future studies will aim to refine the algorithms further, exploring additional variables that may affect breast cancer risk. These could include environmental factors, hormonal influences, and lifestyle modifications. As data collection becomes increasingly sophisticated, the potential to incorporate an even broader range of influences into predictive models continues to expand.
Furthermore, collaboration across disciplines will be critical in advancing this research. Engaging experts from fields such as epidemiology, radiology, and genomic research can foster a more holistic understanding of breast cancer and the factors influencing its development. By promoting interdisciplinary collaboration, researchers can generate insights that may lead to even more nuanced approaches to breast cancer prediction and prevention.
As the research continues to gain attention, the broader implications of integrating artificial intelligence into medical diagnostics are becoming clear. The potential for such models to offer rapid, accurate assessments could revolutionize not only breast cancer diagnosis but also a wide array of other medical fields. The benefits of AI in healthcare are being recognized, suggesting that this is just the beginning of a wider transformation in how diseases are detected and treated.
The integrated model serves as a beacon of hope for many women and their families. Its multifaceted approach towards early breast cancer prediction signifies a turning point in how we conceptualize and address cancer from a preventative standpoint. With early detection being paramount in saving lives, research such as this shines a light on the path forward, advocating for strategies that empower women with knowledge and options in navigating their health journeys.
In conclusion, the advent of this integrated model presents an exciting chapter in the ongoing fight against breast cancer. As the healthcare landscape evolves and embraces innovative technologies, the role of early prediction becomes increasingly critical. Sreelekshmi, Pavithran, and Nair’s work not only demonstrates the power of integrating patient data with imaging diagnostics but also fosters a culture of proactive health management. Their contributions underscore a vital message: early detection through innovative approaches can lead to not just better outcomes but also a fundamentally human-centered approach to health.
This essential research could ultimately prove to be a catalyst for change, igniting further studies and advancements in breast cancer detection methodologies. By fostering ongoing dialogue about the importance of early detection, researchers can encourage women to take proactive steps toward their health. By utilizing insights like those from this integrated model, we may finally be on the verge of turning the tide in the fight against breast cancer.
Subject of Research: Early breast cancer prediction using microcalcifications and patient risk factors.
Article Title: An integrated model for early breast cancer prediction using microcalcifications and patient risk factors.
Article References: Sreelekshmi, V., Pavithran, K. & Nair, J.J. An integrated model for early breast cancer prediction using microcalcifications and patient risk factors. Discov Artif Intell 6, 30 (2026). https://doi.org/10.1007/s44163-025-00775-y
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s44163-025-00775-y
Keywords: Breast cancer, microcalcifications, patient risk factors, early prediction, artificial intelligence, healthcare innovation.
Tags: advancements in breast cancer researchbridging gaps in breast cancer detectioncomprehensive approaches to cancer diagnosisearly breast cancer detectiongenetic predispositions and breast cancerimportance of early intervention in breast cancerinnovative cancer prediction modelsmammogram limitations in breast cancer diagnosismicrocalcifications and breast cancerpatient risk factors for cancerpersonalized risk assessments for womenpredictive accuracy in cancer detection