Renal cell carcinoma (RCC) poses a significant challenge for the medical community, as it stands as one of the most prevalent types of kidney cancer. With traditional treatment methods often leading to varied outcomes among patients, there is an acute need for innovative approaches in cancer treatment. To address this, a recent study has emerged that examines the potential of renal cell carcinoma organoids as a vital component in the development of precision medicine. The study navigates the intricate relationship between models and actual patient outcomes in a groundbreaking manner.
Researchers have developed renal cancer organoids to mimic the actual tumor environment, thereby providing a powerful tool for understanding the disease. Cultivating these miniature versions of tumors allows scientists to investigate how different cancer cells react to various treatments in a controlled environment. This dynamic approach emphasizes the dire need for personalized therapies, as it underscores the importance of patient-specific tumor responses rather than relying solely on standard treatment protocols.
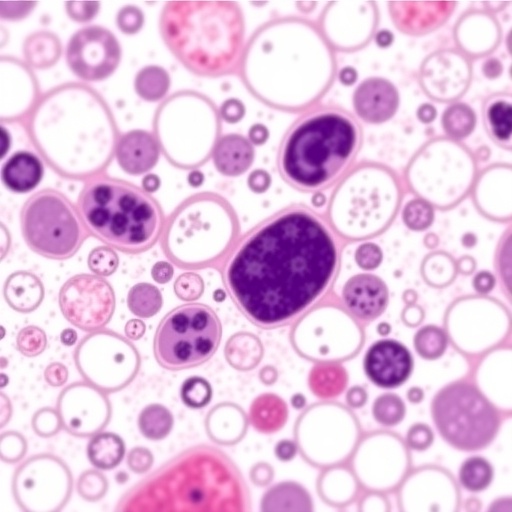
The technology behind organoids is advanced, leveraging stem cell biology to create three-dimensional structures that reflect the original tumor’s architecture and cellular composition. This takes cancer research beyond traditional cell lines and two-dimensional cultures, offering a more accurate representation of the tumor microenvironment. Such advancements open the door for treatments that are tailored to the unique genetic makeup of each patient’s cancer, potentially leading to higher success rates in therapies.
The study highlights how these organoids can serve as testing grounds for various pharmaceutical compounds. By deploying a library of cancer drugs on multiple organoid models, researchers can observe which medications are effective for which tumor profiles. This not only informs drug selection for individual patients but may also lead to the discovery of novel therapeutic agents that can be introduced into the clinical arsenal against renal cell carcinoma.
Furthermore, the implications of utilizing organoids extend beyond drug testing. The integration of these models into clinical practice means better monitoring of treatment responses. As patients undergo therapy, their tumors could be biopsied, and organoids created from these fresh samples. This could facilitate real-time adjustments to treatment regimens based on how the tumor evolves and responds to therapy. This ongoing dialogue between models and patient data has the potential to revolutionize cancer management.
Much of the promise surrounding organoid technology is its capability to reflect the heterogeneity of tumors. RCC is notorious for its complexity and diversity, often exhibiting a wide range of genetic mutations across different patients. By employing organoids that encapsulate this diversity, researchers can better appreciate the nuances of tumor behavior and treatment responses.
Moreover, the ethical considerations of organoid research cannot be overlooked. By using organoids derived from patients, the ethical implications are significantly reduced compared to traditional animal models. These mini-tumors allow researchers to investigate human-specific responses to treatments, creating a more ethical landscape for cancer research while still adhering to the rigor required in scientific exploration.
Despite the excitement surrounding organoids, there remain several challenges to overcome before these models can be universally adopted in clinical settings. Standardization of organoid culture protocols is crucial to ensuring reproducibility of results. Furthermore, there is an urgent need for broader validation studies that establish the correlation between organoid responses and actual patient outcomes.
In addition to these practical challenges, there is also an educational component to this technological shift. Healthcare providers will need to be trained on how to interpret organoid results and incorporate them into treatment plans effectively. Bridging the gap between laboratory research and clinical application is essential to ensure that patients receive the benefits of this innovative approach.
Furthermore, as organoid technology continues to evolve, the potential for integrating cutting-edge techniques such as CRISPR-Cas9 gene editing offers exciting possibilities for future research. This can allow scientists to modify organoids to study specific genetic mutations that drive renal cell carcinoma, tailoring treatment approaches even further.
In conclusion, the research surrounding renal cell carcinoma organoids marks a pivotal point in the evolution of precision medicine. By bringing together models closely resembling actual tumors and the patients from whom they are derived, we are moving towards a future of tailored therapies that promise to enhance the efficacy of treatments while minimizing adverse effects. As this field advances, it is imperative that researchers remain committed to addressing the challenges ahead, ensuring that the remarkable potential of organoids translates into real-world benefits for patients battling renal cell carcinoma.
Subject of Research: Renal cell carcinoma organoids for precision medicine
Article Title: Renal cell carcinoma organoids for precision medicine: bridging the gap between models and patients
Article References:
Gao, J., Luo, H., Wang, S. et al. Renal cell carcinoma organoids for precision medicine: bridging the gap between models and patients. J Transl Med 23, 1152 (2025). https://doi.org/10.1186/s12967-025-06949-7
Image Credits: AI Generated
DOI: 10.1186/s12967-025-06949-7
Keywords: renal cell carcinoma, organoids, precision medicine, cancer research, tumor microenvironment, drug testing, personalized therapies, genetic makeup, CRISPR-Cas9.
Tags: advanced cancer research methodologieskidney cancer treatment innovationsorganoid technology in oncologyovercoming challenges in kidney cancer therapypatient-specific cancer treatment strategiespersonalized cancer therapies developmentprecision medicine in renal cell carcinomarenal cell carcinoma organoids researchstem cell technology in cancer treatmentthree-dimensional tumor modelstumor microenvironment modelingunderstanding cancer cell responses