For the 314,000 people diagnosed with ovarian cancer each year, hope often comes in the form of platinum-based drugs such as cisplatin.
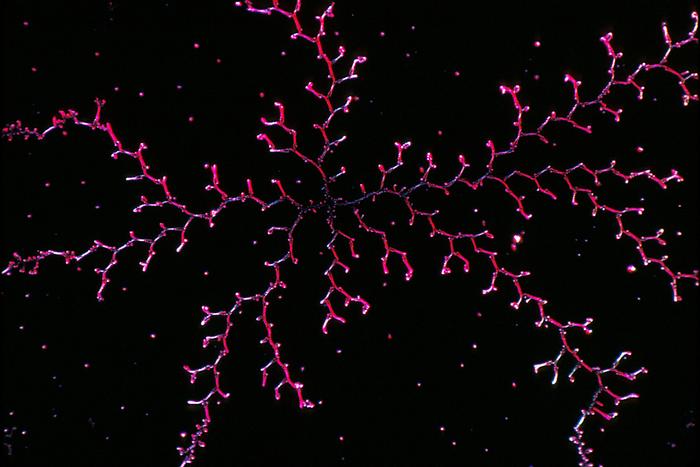
Credit: Larry Ostby, National Cancer Institute
For the 314,000 people diagnosed with ovarian cancer each year, hope often comes in the form of platinum-based drugs such as cisplatin.
Cisplatin causes the death of quick-dividing tumour cells, so it is a potent first-line defence in the treatment of the often fatal disease.
However, over half of ovarian cancer patients develop recurrence and become resistant to cisplatin and other platinum-based chemotherapies, contributing to the five-year survival rate of 31%.
It is unclear why this resistance occurs, but a solution is urgently needed.
In a recent study published in the journal Cancer Gene Therapy, a team of researchers from China and the UK were able to reduce the growth of cisplatin-resistant tumours in female mice by decreasing the activity of a gene called superoxide dismutase 1 (SOD1).
SOD1 is an important tool in the body’s attempts to protect itself and reduce cell damage. However, in some cases, SOD1 levels may become too high and be detrimental.
SOD1 off!
The study extends previous work on ovarian cancer cells that showed cisplatin-resistant tumour cells had high levels of SOD1 as a result of damage induced by cisplatin treatment side effects. The results suggested that reducing SOD1 levels can stop cells from becoming resistant to the chemotherapeutic drug.
The use of small-interfering RNA (siRNA), a class of molecules that can control the expression of genes, can decrease SOD1 expression levels. However, the delivery of siRNA into the body has several problems as it degrades quickly and is unable to reach its target before the kidneys filter it out.
In this latest research, the team developed a method using nanoparticles to deliver siRNA to the target tumour tissue in mice without it being degraded so quickly.
The results showed that when the siRNA was successfully transported and released into tumour tissue six times over 14 days in female mice, the tumour showed reduced growth and decreased resistance to cisplatin.
Therefore, the researchers confirmed SOD1 as a suitable target for overcoming cisplatin resistance.
Professor Mu Wang, from Xi’an Jiaotong-Liverpool University, China, and the corresponding author of the paper, says: “Compared with the control group of mice that did not receive the injection of nanoparticles with siRNA, the mice that received two doses had enhanced sensitivity to cisplatin treatment without obvious physiological toxicity.”
Targeting delivery
To deliver the siRNA to the tumour tissue, the team injected female mice with nanoparticles made out of graphene oxide. The siRNA was contained within the nanoparticles, which have been successful as siRNA carriers in other studies.
In this work, however, the graphene oxide nanoparticles caused some toxicity and liver damage in the mice. The nanoparticles also undid some of the positive effects of using siRNA to reduce SOD1 levels, as the nanoparticles themselves caused an increase in SOD1.
The researchers were able to decrease some of the toxicity by modifying the nanoparticles.
Now that the team have identified the potential of targeting SOD1 to reduce cisplatin resistance and shown that the siRNA for SOD1 itself has limited toxicity, they will continue to investigate the full extent of reducing SOD1 levels and explore other siRNA delivery methods to carry it to the targeted tumour tissue.
Professor Wang says: “We hope this result will provide new ideas and important scientific references for clinical exploration to overcome tumour cisplatin resistance and the drug resistance problem that has plagued ovarian cancer chemotherapy for a long time will hopefully be resolved.”
Journal
Cancer Gene Therapy
DOI
10.1038/s41417-023-00659-2
Method of Research
Experimental study
Subject of Research
Animals
Article Title
Targeting SOD1 via RNAi with PEGylated graphene oxide nanoparticles in platinum-resistant ovarian cancer
Article Publication Date
15-Aug-2023
COI Statement
The authors declare no competing interests.



