In recent years, the field of medical reconstruction has witnessed a transformative revolution, particularly within the realm of mandibular surgery. The traditional approaches, which often yielded unsatisfactory results and involved protracted recovery periods, have gradually been supplanted by pioneering techniques that personalize reconstructive solutions. A recent study underscores the efficacy of in-house patient-specific solutions for mandibular reconstruction, revealing significant advancements aimed at enhancing surgical outcomes and improving patient satisfaction.
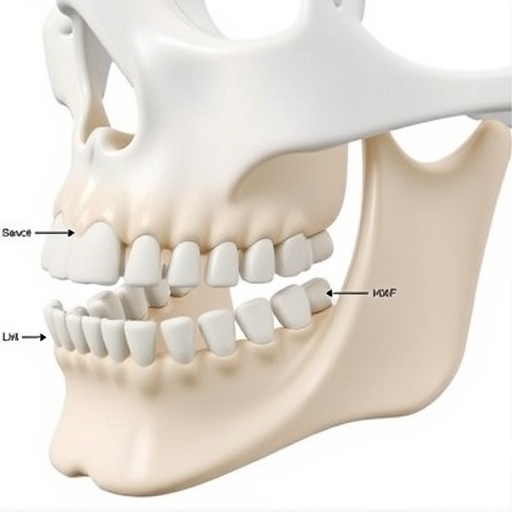
At the heart of this study is the methodology utilized for creating patient-specific mandibular models, which have dramatically altered the landscape of reconstructive surgery. The researchers developed detailed three-dimensional (3D) models derived from CT imaging, meticulously tailored to reflect the unique anatomical features of each patient’s mandible. This pre-surgical planning tool has enabled surgeons to foresee potential challenges and customize interventions, leading to smoother and more efficient surgical procedures.
One of the essential advances highlighted in this research is the use of advanced 3D printing technologies. These technologies enable the fabrication of accurate models and prosthetics that mirror the exact dimensions and structural nuances of the patient’s jaw. By employing biocompatible materials, surgeons can create constructs that not only fit seamlessly but also integrate biologically with the surrounding tissues. This compatibility plays a crucial role in the healing process, helping to expedite recovery times and reduce the risk of complications.
The study also emphasizes the collaborative aspect of the reconstruction process. The incorporation of a multidisciplinary team, including surgeons, radiologists, and biomedical engineers, has proven advantageous. This collaboration fosters an environment where shared expertise leads to improved problem-solving and innovation. By working together, the team is able to address each patient’s unique challenges, resulting in tailored surgical plans that cater specifically to individual needs.
Patient outcomes have shown remarkable improvement as a result of these innovations. The researchers reported a reduction in postoperative complications, with patients experiencing fewer instances of infection or implant failure. Furthermore, the use of these patient-specific solutions has led to shorter hospital stays and quicker return to normal activities, significantly enhancing the overall patient experience.
Additionally, the psychological impact of personalized solutions cannot be overstated. Many patients reported increased satisfaction with their reconstruction outcomes, which directly correlates to improved psychosocial well-being. Reconstructive surgery often comes with emotional weight, as patients seek to regain not just functionality but also their sense of identity. The ability to produce aesthetically pleasing results that align closely with the patient’s original anatomy plays a pivotal role in achieving these emotional and psychological goals.
The implications of this research extend beyond individual patient care; they hint at future possibilities for broader medical applications. The principles established in mandibular reconstruction can potentially be extrapolated to other areas of surgical intervention, including craniofacial reconstruction and orthopedic surgery. As technology continues to advance, the potential for in-house customization could redefine standard surgical practices across various medical fields.
Despite these advancements, the research team acknowledges that challenges remain. The initial cost of producing patient-specific models and the required technical expertise can pose barriers, particularly in resource-limited settings. However, the potential long-term savings associated with reduced complications and shorter recovery times present a compelling argument for investment in these technologies.
In addition to cost considerations, there is a need for ongoing research to refine these methods further. The study opens doors for investigating different materials and techniques that could enhance the biocompatibility and longevity of the implants used. Understanding the biological interactions that occur post-implantation remains vital for ensuring sustained success in reconstructive surgery.
Furthermore, ethical considerations around patient data and consent in the context of personalized medicine must be addressed. As surgical techniques become more tailored, conversations surrounding patient privacy, data security, and the ethical implications of using personalized 3D models will become increasingly important.
Ultimately, the findings from this study pave the way for a new era in reconstructive surgery. The transition from one-size-fits-all approaches to personalized, patient-centered care represents a significant milestone in the medical field. It holds the promise of not only restoring physical form and function but also enhancing the psychological and emotional well-being of patients.
As we continue to explore the intersection between technology and medicine, the pursuit of improved surgical outcomes remains at the forefront. The breakthroughs reported here signal that the future of mandibular reconstruction—and indeed, reconstructive surgery as a whole—looks increasingly bright, with patient-centric innovations leading the charge.
The ongoing dialogue around these advancements will be critical, fostering an environment of collaboration and continuous improvement. As we stand on the brink of a future where personalized medicine becomes the norm, the lessons learned from mandibular reconstruction will undoubtedly inform practices across diverse medical domains, ultimately benefiting patients worldwide.
Subject of Research: Mandibular Reconstruction Outcomes for In-House Patient-Specific Solutions
Article Title: Mandibular reconstruction outcomes for in-house patient-specific solutions
Article References:
Marquardt, M., Cowen, E., Fenberg, R. et al. Mandibular reconstruction outcomes for in-house patient-specific solutions. 3D Print Med 11, 31 (2025). https://doi.org/10.1186/s41205-025-00280-z
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s41205-025-00280-z
Keywords: Mandibular Reconstruction, Patient-Specific Solutions, 3D Printing, Surgical Outcomes, Personalized Medicine, Biocompatibility, Multidisciplinary Approach.
Tags: 3D modeling in surgeryadvanced 3D printing technologiesanatomical modeling for surgerybiocompatible materials in prostheticsCT imaging for reconstructive surgerycustom interventions in mandibular surgeryenhancing surgical outcomesimproving recovery in mandibular reconstructionpatient satisfaction in surgerypatient-specific surgical solutionspersonalized mandibular reconstructionreconstructive surgery innovations