In recent years, the field of healthcare has witnessed a significant shift towards patient-centered care, particularly in countries like China. A groundbreaking study conducted by Yin, Gao, Cui, and their colleagues seeks to unravel the complexities surrounding patient and healthcare professional preferences within the sphere of integrated care. The researchers utilized a unique best-worst scaling methodology for this comparative analysis, a technique gaining traction for its ability to capture nuanced preferences more effectively than traditional survey methods. The study’s findings promise to shed light on the disparities and alignments between patients and healthcare providers when it comes to the ideals of patient-oriented health services.
Patient-centered care is a cornerstone of modern healthcare practices, emphasizing the importance of tailoring healthcare services to meet the individual needs and preferences of patients. In China, where the healthcare system is grappling with challenges such as rapid population aging and increasing chronic disease prevalence, understanding the preferences of both patients and healthcare professionals is critical. The insights garnered from this research can inform policy-making and improve the overall quality of care delivered to patients in various healthcare settings across the nation.
To conduct this research, the authors employed a robust methodology that involved gathering quantitative data through best-worst scaling. This approach allowed participants to evaluate multiple attributes of integrated care by selecting the ‘best’ and ‘worst’ aspects of their experiences. By doing so, the study not only highlighted the most valued elements of patient-centered care but also illuminated which factors were deemed less important. This dual insight is invaluable for shaping future healthcare policies and practices in China, where the demand for high-quality, responsive care is on the rise.
One of the intriguing aspects of the study was the recruitment of a diverse cohort of participants that included both patients and healthcare professionals from various specialties. This inclusivity enriches the study’s findings, allowing for a broader perspective on patient care preferences. Additionally, the diversity adds layers to understanding the complex dynamics at play in the Chinese healthcare environment. By carefully analyzing feedback from both demographics, the research team was able to uncover contrasts and similarities that illuminate the shared goals and unique priorities of patients and healthcare providers alike.
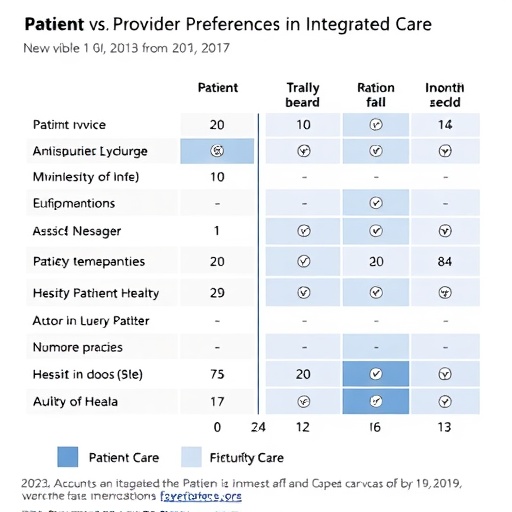
The findings of this comparative analysis indicate that, while there are many shared values, distinct preferences do exist between patients and healthcare professionals regarding integrated care. For instance, patients may prioritize accessibility and emotional support as critical components of their healthcare experiences, while healthcare providers may place a higher emphasis on clinical outcomes and operational efficiency. Understanding these preferences is crucial for designing integrated care models that satisfy both parties, thus fostering a more collaborative environment that benefits health outcomes.
Furthermore, the implications of this research extend beyond academic interest; they hold potential ramifications for health policy formulation. Policymakers can utilize these insights to enhance integrated care strategies, ensuring that they are aligned with both patient desires and healthcare professional capabilities. As China continues to reform its healthcare system, integrating feedback from both patients and providers will be essential in developing comprehensive policies that ensure sustainable and effective healthcare delivery.
In light of the ongoing transition toward integrated care models, the study underscores the importance of adopting a collaborative approach in healthcare settings. By fostering open communication between patients and healthcare professionals, the chances of developing care plans that accurately reflect patient needs are significantly enhanced. The results of this study can guide training programs for healthcare professionals to better understand and appreciate the perspectives of their patients, ultimately leading to a more patient-centric healthcare landscape.
Additionally, the study reveals potential areas for future research. Understanding the cultural and contextual factors that influence patient and provider preferences can provide deeper insights into how integrated care can be effectively implemented across different regions in China. Future studies might delve into the impact of socioeconomic status, urban vs. rural healthcare disparities, and the role of technology in shaping expectations and experiences. These avenues of exploration could further refine the understanding of integrated care within the evolving landscape of Chinese healthcare.
This research represents a necessary step in bridging the gap between patient preferences and healthcare professional practices. By emphasizing collaboration and mutual understanding, it illuminates the path toward a more integrated and responsive healthcare system. The findings advocate for actionable strategies to enhance communication and partnership between patients and providers, strengthening the foundation of patient-centered care in China.
In conclusion, the study by Yin and colleagues is not merely an academic exercise; it serves as a clarion call for a more attentive and inclusive approach to healthcare provision. As the healthcare landscape continues to evolve, the voices of both patients and providers must be recognized and valued, ensuring that the future of healthcare is built on a solid foundation of mutual respect and understanding.
With the rapid advancement of healthcare practices, studies like this one are vital in guiding stakeholders toward creating a more integrated and patient-oriented system. Ultimately, the goal is to foster an environment where healthcare decisions are made collaboratively, leading to improved health outcomes for all segments of the population.
This comprehensive analysis contributes to an expanding body of literature that seeks to understand and harness patient and provider preferences in delivering quality care. By highlighting where interests align and diverge, it lays essential groundwork for future innovations in healthcare delivery, emphasizing that the best patient care arises from uniting the expertise of healthcare professionals with the insights of those they serve.
As this research makes its way into policy-making discussions and healthcare practices in China, it stands to reshape how integrated care is conceptualized and operationalized, with the potential for broader implications in the global discourse on patient-centered healthcare.
Subject of Research: Preferences for Patient-Centered Integrated Care in China
Article Title: Comparing patient and healthcare professional preferences for patient-centered integrated care in China: a best-worst scaling study
Article References:
Yin, Y., Gao, W., Cui, X. et al. Comparing patient and healthcare professional preferences for patient-centered integrated care in China: a best-worst scaling study.
BMC Health Serv Res (2026). https://doi.org/10.1186/s12913-025-13957-2
Image Credits: AI Generated
DOI: 10.1186/s12913-025-13957-2
Keywords: Patient-Centered Care, Integrated Care, Healthcare Preferences, China, Best-Worst Scaling, Health Policy.
Tags: aging population healthcare challengesbest-worst scaling methodologychronic disease management in Chinahealthcare policy implicationshealthcare provider perspectivesimproving healthcare quality in Chinaintegrated care preferencespatient satisfaction metricspatient-centered healthcarepatient-provider alignmentqualitative research in healthcaretailoring healthcare services