The intricacies of pain have baffled scientists and physicians for centuries, evolving from being perceived merely as a fleeting sensory experience to a profound, lasting state enmeshed within the entire brain and body. Contemporary neuroscience embraces this paradigm shift—pain is no longer understood as a momentary signal but as a persistent condition reflecting complex neurophysiological and behavioral dynamics. Fully deciphering this enduring pain state, particularly in preclinical models, is imperative for developing novel therapeutic interventions that address not just acute discomfort but the deeper, chronic experience that afflicts millions globally.
Traditional behavioral assessment methods for pain, which typically rely on external responses to nociceptive stimuli, have proven insufficient. Pain states endure long after outward coping behaviors cease, suggesting that underlying neural mechanisms maintain an internal, ongoing experience independent of immediate stimuli. To bridge this gap, researchers have innovated more objective and unbiased computational approaches to decode subtle indicators of pain states. These advances include sophisticated analyses of posture, facial expression metrics, and now, neurophysiological signatures alongside control theory behavioral modeling, which together afford a more comprehensive lens into the persistence of pain.
Recent groundbreaking work elucidates the role of a specific subset of neurons within the lateral parabrachial nucleus (lPBN), distinguished by their expression of the neuropeptide Y receptor type 1 (Y1R), as critical mediators of prolonged pain states. Unlike direct responses to acute noxious inputs, these Y1R-expressing neurons exhibit sustained activity long after injury, indicating their involvement in the central encoding of chronic pain. This functional persistence in the absence of external harmful stimuli points towards complex plastic changes involving peripheral nervous system sensitization and central neural network remodeling.
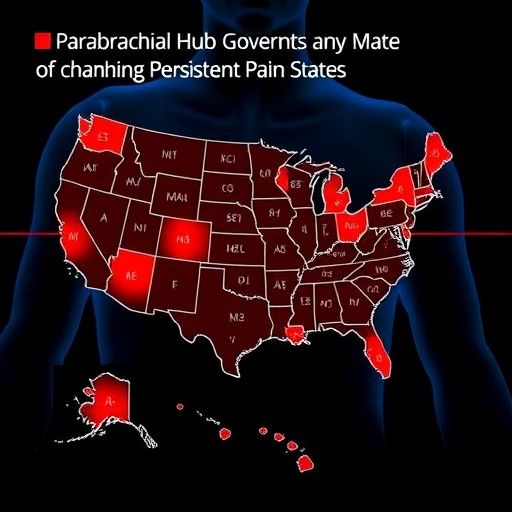
The PBN itself is a pivotal hub receiving spinal nociceptive projections, positioning Y1R neurons strategically to integrate diverse sensory inputs. Notably, these neurons are widely distributed both molecularly and spatially across the known subdivisions and neuronal populations within the PBN, an arrangement that underpins their capacity to orchestrate multifaceted pain-related processes. The expression of Y1 receptors in roughly one-fifth of neurons associated with pain modulation highlights the extensive reach and influence of this ensemble, which appears less dedicated to coding acute painful stimuli and more adept at monitoring sustained affective and coping-related changes post-injury.
Such distribution confers upon Y1R neurons in the PBN a sentinel-like function that transcends simple nociception, capturing the ongoing internal state of distress and pain affect. This integrative role aligns with parallels drawn to Y1R-expressing neurons within other brain regions such as the hypothalamus, which are known to govern essential physiological states and adaptive behaviors. The multidimensional nature of these neurons enables not only the monitoring of pain but also its modulation through convergent signaling pathways activated by physiological needs and environmental inputs.
The authors of this study reveal that endogenous analgesic mechanisms leverage this circuitry to dynamically suppress chronic pain by gating the pain signal at the level of the PBN through neuropeptide Y (NPY) signaling pathways. This neuromodulatory action appears finely tuned, allowing survival-driven needs—such as hunger, thirst, or reproductive drives—to transiently override persistent pain sensations. This prioritization reflects a sophisticated evolutionary adaptation enabling organisms to shift cognitive resources away from pain toward behaviors critical for immediate survival.
Importantly, this gating does not appear to influence acute nociceptive responses, underscoring a functional dissociation between the processing of immediate pain threats and longer-lasting pain states. By tuning the integration of nociceptive inputs, Y1R neurons modulate behavioral outputs selectively during chronic phases, suggesting a targeted, state-dependent gate that can recalibrate the pain experience without disrupting essential protective reflexes.
The discovery of this parabrachial hub as a confluence point for the control of enduring pain opens promising pathways for therapeutic innovation. Pharmacological or behavioral therapies designed to selectively activate or mimic Y1R neuron signaling could offer potent relief for chronic pain sufferers without the drawbacks of globally dampening sensory perception or the risks associated with opioid therapies. This focused approach promises higher efficacy coupled with fewer side effects.
Future research directions emphasize expanding the characterization of the molecular and circuit-level mechanisms underlying Y1R neuron function, as well as exploring their interaction with other neuromodulatory systems implicated in pain and homeostatic regulation. Additionally, preclinical experimentation must probe how environmental and physiological variables can harness this intrinsic analgesic circuit to develop non-invasive treatment modalities.
Considering the vast impact of long-term pain on quality of life and the limitations of current analgesics, these findings represent a seismic shift in pain neuroscience. By revealing how endogenous systems prioritize survival needs over pain perception, this work redefines the conceptual framework of pain management and lays the groundwork for transformative clinical strategies aimed at chronic pain relief.
In sum, this research articulates a nuanced, integrative pain control architecture centered on Y1R-expressing neurons in the lateral parabrachial nucleus. It highlights how a convergence of neurophysiological monitoring, adaptative gating, and behavioral modulation collaborate to sustain or diminish the experience of enduring pain in response to competing survival demands, offering an exciting frontier in pain biology and therapeutics.
Subject of Research: Neural mechanisms and circuits underlying the regulation of persistent pain states by Y1 receptor-expressing neurons in the lateral parabrachial nucleus.
Article Title: A parabrachial hub for need-state control of enduring pain.
Article References:
Goldstein, N., Maes, A., Allen, H.N. et al. A parabrachial hub for need-state control of enduring pain. Nature (2025). https://doi.org/10.1038/s41586-025-09602-x
Image Credits: AI Generated
Tags: behavioral indicators of painchronic pain neurosciencecomputational pain analysis techniquesinnovative pain research methodologieslateral parabrachial nucleus functionneural mechanisms of pain persistenceneurophysiological pain assessmentobjective pain measurement strategiespersistent pain mechanismspreclinical models of pain studytherapeutic interventions for chronic painunderstanding pain as a condition