In a groundbreaking development that merges cutting-edge artificial intelligence with noninvasive diagnostic medicine, researchers have unveiled a novel model capable of screening chronic kidney disease (CKD) and identifying its common pathological subtypes through analysis of retinal images. This innovative approach holds the potential to revolutionize CKD detection and monitoring, offering a painless, accessible, and cost-effective alternative to conventional invasive methods. Given the substantial burden of CKD worldwide, which often advances silently until severe dysfunction occurs, early and precise diagnosis is paramount. The newly introduced model leverages retinal microvascular features as biomarkers, illuminating the intimate connection between kidney health and retinal vasculature.
The study, published in Nature Communications, presents an AI-powered framework trained on a vast and diverse dataset of retinal fundus photographs paired with clinical records. By harnessing advanced deep learning algorithms, the model effectively bridges the gap between ophthalmic imaging and nephrology, yielding a tool that not only screens for CKD but also discriminates among its prevalent pathological types. This dual functionality marks a significant leap beyond traditional diagnostic paradigms, which commonly rely on blood and urine tests, imaging modalities, or biopsy, each with inherent limitations relating to invasiveness, accessibility, or expense.
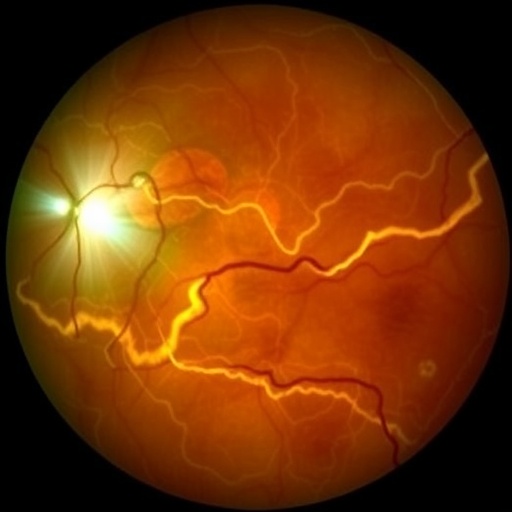
At the heart of the methodology lies a sophisticated convolutional neural network (CNN) architecture meticulously designed to extract subtle vascular and structural patterns associated with renal impairment from retinal images. The retina, a uniquely accessible window into the microcirculation, mirrors systemic vascular alterations that correlate with kidney pathology. By detecting and quantifying these microvascular changes—such as vessel caliber, tortuosity, and hemorrhages—the AI system infers the presence and severity of CKD with remarkable accuracy. Notably, the model’s capacity to discern pathological subtypes, including diabetic nephropathy, hypertensive nephrosclerosis, and glomerulonephritis, stems from its ability to identify distinctive retinal vascular signatures linked to each condition.
.adsslot_RpLF0gJEis{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_RpLF0gJEis{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_RpLF0gJEis{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
The research team compiled an extensive dataset comprising over tens of thousands of retinal images annotated with corresponding renal function indices and histopathological diagnoses. To ensure robustness and generalizability, the dataset encompassed multiethnic populations across various geographic regions, accounting for heterogeneity in disease presentation and comorbidities. Training involved cross-validation protocols and rigorous hyperparameter tuning to optimize predictive performance while minimizing overfitting. Additionally, the researchers incorporated explainability mechanisms to elucidate the model’s decision pathways, enabling clinicians to interpret how retinal features influence diagnostic predictions.
One of the most compelling aspects of this model is its noninvasive nature. Traditional diagnostic workflows for CKD often require blood draws to measure serum creatinine, urine collection for albuminuria assessment, and at times, renal biopsies that carry procedural risks. In contrast, retinal imaging is a quick, painless, and widely available modality routinely performed in ophthalmologic settings. By integrating CKD screening into retinal examinations, the model offers a pathway for opportunistic and large-scale population screening, especially beneficial in resource-limited settings or for patients reluctant to undergo invasive testing.
The implications for healthcare delivery are profound. Early identification of CKD and its pathological drivers enables timely interventions that slow disease progression and reduce cardiovascular and renal complications. The model’s ability to stratify pathological types further supports personalized medicine by guiding targeted therapeutic strategies and monitoring treatment response. Moreover, this technology could democratize CKD screening on a global scale, addressing disparities in access to specialty nephrology care and improving outcomes through proactive management.
Beyond clinical utility, the study also demonstrates the broader potential of retinal imaging as a biomarker reservoir for systemic diseases. The fine-grained microvascular alterations captured in retinal photographs carry diagnostic and prognostic information not limited to the eye but reflective of the body’s vascular health. This paradigm underscores the convergence of ophthalmology and internal medicine, facilitated by machine learning tools, fostering interdisciplinary innovation.
Validation analyses underscored the model’s high sensitivity and specificity in detecting CKD across early and advanced stages, surpassing several existing noninvasive screening tools. Importantly, subgroup analyses revealed consistent performance irrespective of demographic variables such as age, sex, and ethnicity, signifying the model’s applicability across diverse patient populations. The authors also highlighted the potential for integration into mobile retinal imaging devices and telemedicine platforms, which could expand reach to underserved communities.
While promising, the researchers acknowledge challenges ahead before clinical implementation. Prospective studies are needed to further assess the model’s predictive accuracy in real-world settings and to understand the longitudinal relationship between retinal vascular changes and kidney disease evolution. Additionally, regulatory clearances, data privacy considerations, and clinician training will play critical roles in translating this innovation to bedside practice.
The fusion of AI and retinal imaging heralds a new era in CKD management, shifting focus toward preventative nephrology underscored by precision screening. This approach holds promise not only in mitigating the global CKD burden but also in stimulating future research exploring retinal biomarkers in other chronic conditions. As the medical community grapples with escalating incidences of renal diseases, such transformative technologies may pave the way toward earlier, less invasive, and more personalized care.
The integration of this model into routine retinal imaging workflows is particularly timely given increasing prevalence of diabetes and hypertension—primary drivers of CKD—thus setting the stage for a public health breakthrough. By shifting CKD detection from reactive to proactive, it empowers earlier intervention that can stem progression to end-stage renal disease, ultimately transforming patient trajectories.
Looking forward, this work lays a foundational framework from which further AI-enhanced multimodal diagnostics could emerge, incorporating genetic, biochemical, and imaging data. The convergence of such datasets may unlock even deeper understanding of CKD pathogenesis and further refine individualized treatment paradigms.
In summary, the noninvasive AI model for chronic kidney disease screening represents a landmark advance marrying ophthalmic imaging and nephrology. With compelling evidence supporting its diagnostic and subclassification capabilities, this technology offers a new horizon in early disease recognition. It exemplifies the disruptive potential of AI in medicine where novel biomarkers gleaned from common clinical images transcend traditional specialty boundaries, ushering in an era of more accessible and effective healthcare.
Subject of Research: Chronic kidney disease (CKD) screening and pathological subtype identification using retinal imaging and artificial intelligence.
Article Title: A noninvasive model for chronic kidney disease screening and common pathological type identification from retinal images.
Article References:
Wu, Q., Li, J., Zhao, L. et al. A noninvasive model for chronic kidney disease screening and common pathological type identification from retinal images. Nat Commun 16, 6962 (2025). https://doi.org/10.1038/s41467-025-62273-0
Image Credits: AI Generated
Tags: advanced deep learning algorithms in healthcareartificial intelligence in medical diagnosticsbridging ophthalmology and nephrologychronic kidney disease subtypes identificationcost-effective kidney disease diagnosisearly diagnosis of chronic kidney diseaseinnovative approaches in chronic disease monitoringNature Communications study on CKD detectionnoninvasive kidney disease detectionpainless alternatives to invasive kidney testsretinal imaging for CKD screeningretinal microvascular features as biomarkers