A groundbreaking study by Gao et al. reveals the potential of radiogenomic MRI biomarkers to revolutionize the prediction of glypican-3 (GPC3) expression and the characterization of tumor microenvironments in hepatocellular carcinoma (HCC). This research, published in the Journal of Translational Medicine, promises to spark interest among oncologists and imaging specialists as it uncovers the interplay between imaging technology and molecular biology to enhance cancer diagnostics and therapy tailoring.
Hepatocellular carcinoma presents a formidable challenge due to its complex biological behavior and heterogeneous nature. Current treatment strategies often fall short because they do not consider the tumor’s molecular makeup. GPC3, a heparan sulfate proteoglycan, is an oncofetal protein frequently overexpressed in HCC, implicating it as a potential biomarker for tumor aggression and patient prognosis. The ability to predict GPC3 levels noninvasively could thus provide a significant advantage in managing this aggressive cancer.
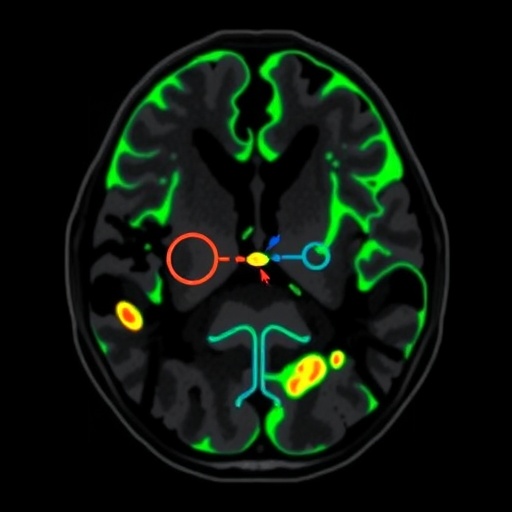
The research team utilized advanced magnetic resonance imaging techniques to identify specific biomarkers associated with GPC3 expression. By correlating the imaging characteristics with histopathological features, the study delineates a pathway where MRI can serve as a non-invasive method to infer not just the presence of tumors, but their underlying biological behavior. This innovative approach could significantly alleviate the need for invasive biopsies, minimizing patient discomfort and risk.
In this study, the authors employed radiogenomics, integrating genomic data with radiological imaging, to unravel how imaging phenotypes can reflect molecular alterations in the tumor microenvironment. This innovative methodology represents a paradigm shift in how oncologists approach diagnosis and treatment for HCC, taking into account both the structural and functional aspects of tumors. The precision obtained through such an approach indicates that personalized medicine could be more achievable in oncology than previously thought.
The researchers meticulously analyzed MRI data from a cohort of HCC patients, employing machine learning algorithms to enhance the predictive power of the identified radiogenomic biomarkers. They found that specific imaging features were significantly associated with high GPC3 expression. These findings suggest that artificial intelligence can be a valuable ally in oncology, driving forward the frontier of predictive medicine and offering enhanced decision-making tools for clinicians.
Furthermore, the study highlights the significance of the tumor microenvironment in influencing tumor behavior and response to therapy. Understanding how various components of the microenvironment interact with tumor cells, particularly in the context of GPC3 expression, could pave the way for the development of novel therapeutic strategies targeting the tumor ecosystem rather than just the cancer cells themselves. This comprehensive understanding may lead to more effective interventions and improved patient outcomes.
The implications of this study extend beyond mere diagnostic capabilities. With the foundation laid by Gao et al., further research could explore targeted therapies directed at GPC3 and its associated pathways, potentially unlocking new avenues for treatment. The recognition of GPC3 as a therapeutic target could enhance the effectiveness of current treatment modalities and result in more favorable prognoses for patients diagnosed with hepatocellular carcinoma.
In an era where precision medicine is becoming paramount, innovative approaches like the one demonstrated in this study could significantly alter the standard of care in oncology. Noninvasive imaging that resonates with the molecular characteristics of tumors embodies the essence of personalized medicine, where treatment plans are tailored to the unique biological profile of individual patients. This study sets a foundation for future investigations that may refine our understanding of HCC and streamline therapeutic approaches.
In conclusion, Gao et al.’s research heralds a promising future in oncology, particularly for the management of hepatocellular carcinoma. By effectively merging imaging findings with molecular insights, this study not only opens new avenues for noninvasive assessment but also launches a query into how radiogenomic technologies can redefine cancer treatment strategies. As the field of oncology continues to evolve, studies like this will be crucial in shaping a more effective, patient-centered approach to cancer care.
The pressing need for innovation in cancer diagnostics and treatment becomes increasingly evident as research like this illuminates the intricate associations between imaging and genetics. Advancing our understanding of tumors through technologies that combine radiological and genomic data could ultimately lead to breakthroughs that enhance survival rates and quality of life for patients facing hepatocellular carcinoma and other malignancies.
As this field of research develops, continual collaboration between radiologists, oncologists, and molecular biologists will be vital. Translational research presents a challenging but rewarding path, requiring a multidisciplinary effort to translate findings from the lab into clinical practice effectively. This study exemplifies the fruitful intersection of imaging and genomics, and the potential for limitless discovery that lies ahead.
The future of oncological care may very well hinge on innovations like the one presented by Gao et al. With emphasis on patient-centered, personalized medicine, the integration of noninvasive MRI techniques with genomic data stands to create a new standard in the way hepatocellular carcinoma is diagnosed, managed, and treated. The path paved by this research holds promise not just for HCC, but for the entire field of oncology as it embraces the inherent complexity of cancer as a disease.
With ongoing advancements in technology and scientific research, it is essential for healthcare practitioners and researchers to remain engaged with emerging methodologies. Studies focusing on the applications of radiogenomics could catalyze a new era of insightful, individualized cancer treatment by emphasizing the importance of comprehensive tumor profiling. Ultimately, this will contribute not only to improved patient care but also to a more profound understanding of cancer biology.
Subject of Research: Noninvasive prediction of GPC3 expression and tumor microenvironment in hepatocellular carcinoma using MRI biomarkers.
Article Title: Radiogenomic MRI biomarkers for noninvasive prediction of GPC3 expression and tumor microenvironment in hepatocellular carcinoma.
Article References: Gao, Y., Liu, D., Miao, Y. et al. Radiogenomic MRI biomarkers for noninvasive prediction of GPC3 expression and tumor microenvironment in hepatocellular carcinoma. J Transl Med (2025). https://doi.org/10.1186/s12967-025-07504-0
Image Credits: AI Generated
DOI: 10.1186/s12967-025-07504-0
Keywords: radiogenomics, hepatocellular carcinoma, GPC3, MRI biomarkers, tumor microenvironment, noninvasive prediction.
Tags: advanced MRI techniques in oncologyglypican-3 expression predictionGPC3 as cancer biomarkerhepatocellular carcinoma imagingmolecular profiling in HCCnoninvasive cancer management strategiesnoninvasive MRI biomarkersoncological imaging advancementspredictive imaging for tumor aggressionradiogenomics in cancer diagnosticstumor biology and imaging interplaytumor microenvironment characterization