Most chronic wound infections share one thing in common: the presence of biofilms, which are composed of many different microorganisms that congregate as a mass, usually on some type of surface such as a wound bed. Biofilms are thought to be associated with up to 80% of infections, and their ability to stick together makes the biofilm and infection exceptionally difficult to kill.
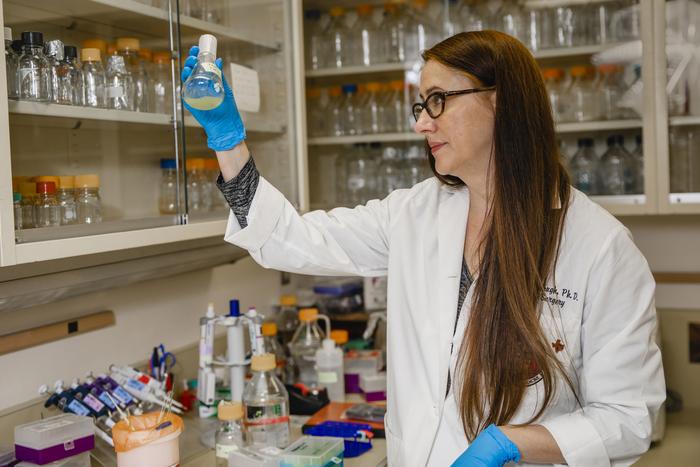
Credit: TTUHSC
Most chronic wound infections share one thing in common: the presence of biofilms, which are composed of many different microorganisms that congregate as a mass, usually on some type of surface such as a wound bed. Biofilms are thought to be associated with up to 80% of infections, and their ability to stick together makes the biofilm and infection exceptionally difficult to kill.
To combat this health care challenge, researchers such as Kendra Rumbaugh, Ph.D., a professor in the Texas Tech University Health Sciences Center (TTUHSC) School of Medicine’s Department of Surgery, are pursuing biofilm dispersal agents such as specific enzymes in hopes the enzymes can induce microbes to leave the safety of the protective biofilm and become more susceptible to antibiotics. Rumbaugh’s efforts received a funding boost in December when she was awarded a two-year, $434,938 grant (“Bacterial and host response to biofilm dispersal in wound infections”) from the National Institute of Allergy and Infectious Diseases at the National Institutes of Health.
Rumbaugh’s lab has for years focused on researching biofilms — specifically, bacterial biofilms — and their role in wound infections. She said biofilms are problematic in many different types of infections, especially chronic infections where theirformation makes the wound’s microbial components exceptionally resistant to treatment. By focusing on wound infections, Rumbaugh’s lab found that when certain types of bacteria (some more than others) get into a wound, they very often will form a biofilm.
“The bacteria and microbes slow down their metabolism and become almost dormant,” Rumbaugh said. “They go to sleep and surround themselves with an extracellular polymeric substance (EPS), a sticky substance that covers them and protects them, and then they just hunker down.”
Even though the bacteria become dormant in the biofilm, Rumbaugh said past research indicates that the immune system knows the bacteria and the biofilm are there, and it’s responding by producing a variety of things that are supposed to kill the bacteria. However, because the bacteria are embedded in this biofilm, none of those things work, which leads to prolonged inflammation and inhibited wound healing.
“The bacteria are inhibiting the wound from closing and healing, and it’s really hard for the immune system to kill them,” Rumbaugh said. “It’s also really hard for antibiotics to kill them for basically the same reason: they’re dormant and they’re covered up in the biofilm.”
With this new grant, Rumbaugh’s lab will use certain enzymes as tools to understand what happens to bacteria when they’re dispersed from a biofilm rather than working to identify a suitable enzyme for commercialization purposes. They also want to investigate the effects that dispersing a quantity of bacteria from a biofilm produces in the host.
Rumbaugh’s lab has for years been examining the enzymes they hypothesized would break up the bonds that are present in the biofilm. Rumbaugh believes these enzymes, called glycoside hydrolases, actually will break up the EPS and uncover the bacteria so it can be killed by antibiotics.
“Using the enzymes is considered a passive method for dispersing bacteria from a biofilm because the bacteria aren’t really participating in an active way,” Rumbaugh explained. “We’re hitting them with an enzyme that breaks up the EPS, and then they’re uncovered. They do move out of the biofilm, but it’s not the bacteria that are initiating the process of dispersal, so we call that passive dispersal.”
There also are active dispersal methods that can induce different signal transduction pathways in bacteria that cause the bacteria to initiate dispersal themselves. In addition, there are many different characterizations of what happens to bacteria when they are dispersed specifically from a wound.
In this grant, Rumbaugh’s lab will compare several passive and active dispersal methods using different chemical signals, enzymes and processes. As they investigate, Rumbaugh said they will attempt to determine what happens to the bacteria during dispersal. Do they become more virulent or more destructive to the host? On the other hand, they also will be investigating what happens to the host (a mouse in this case) and how it responds over time as the bacteria are dispersed and move systematically through the bloodstream of the mouse.
Rumbaugh said there is also some evidence shown by others that dispersal causes bacteria to alter their gene transcription (the process by which a DNA segment is copied into RNA) in ways that then affect their susceptibility to antibiotics. Therefore, her lab also will investigate whether dispersal alters and influences the bacteria’s susceptibility to antibiotics and other drugs based on the dispersal method being employed.
“That’s important to know if you’re banking on the fact that you’re going to be able to kill them with antibiotics,” Rumbaugh said. “This project will provide more of a basic science understanding of bacterial dispersal from biofilms. I also think this information is important if we’re going to have therapeutics that trigger or capitalize on dispersal in some way in the future. We really need to understand exactly what dispersal is doing to the bacteria and what it’s doing to the host. That’s the primary focus of our study in a nutshell.”
###




