In a landmark breakthrough that could radically transform the therapeutic landscape of glioblastoma, researchers have developed novel imidazotetrazine derivatives capable of overcoming one of the most formidable challenges in cancer treatment—resistance to temozolomide. Glioblastoma multiforme (GBM) is the most aggressive and lethal form of brain tumor, notorious for its resistance to conventional chemotherapeutics, particularly temozolomide, which has been the frontline drug for years. The innovative compounds in this study not only circumvent this resistance but also engage dual cell death pathways—ferroptosis and apoptosis—offering a potent, multi-pronged attack on glioblastoma cells.
Temozolomide resistance in glioblastoma remains a pervasive and devastating issue, severely limiting patient survival despite aggressive treatment regimens. This resistance often arises through several molecular mechanisms, such as upregulation of DNA repair enzymes like O6-methylguanine-DNA methyltransferase (MGMT) and alterations in apoptotic signaling pathways. Consequently, the cytotoxic efficacy of temozolomide is blunted, creating an urgent demand for new therapeutic strategies that can either bypass or directly target these resistance mechanisms.
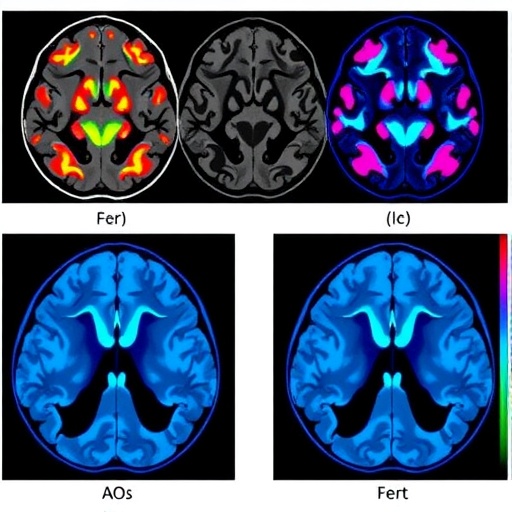
The novel imidazotetrazine derivatives introduced in this study demonstrate a unique ability to induce ferroptosis, an iron-dependent form of programmed cell death characterized by the accumulation of lipid peroxides, alongside apoptosis, the well-known pathway of programmed cell death involving caspase activation. By simultaneously triggering these two mechanisms, the compounds initiate a more comprehensive onslaught on glioblastoma cells, effectively dismantling the cellular defences that confer resistance to temozolomide.
Ferroptosis has drawn tremendous interest in recent years as a promising anticancer strategy, yet its clinical application has been limited by the lack of effective inducers specific to tumor cells. The discovery that these imidazotetrazine derivatives selectively induce ferroptosis in glioblastoma cells is therefore especially significant, opening up new avenues for therapeutic exploitation. This dual induction strategy not only intensifies oxidative stress within tumor cells but also leverages the iron metabolism vulnerabilities unique to cancerous tissues.
The molecular design of the imidazotetrazine derivatives appears to facilitate enhanced tumor penetration and metabolic stability, critical parameters for successful brain tumor therapeutics. Structurally optimized to overcome blood-brain barrier constraints, these compounds maintain high bioavailability within the central nervous system, ensuring potent and sustained pharmacological action. Such properties are essential given the notoriously protective nature of the blood-brain barrier against most chemotherapeutic agents.
Detailed mechanistic studies indicate that upon cellular uptake, these derivatives elevate intracellular iron levels and reactive oxygen species (ROS), leading to the peroxidation of membrane lipids, a hallmark event triggering ferroptosis. Concurrently, the compounds activate key apoptotic mediators including caspase-3 and the mitochondrial apoptotic pathway, resulting in synergistic cytotoxic effects. This sophisticated orchestration disrupts tumor cell homeostasis at multiple checkpoints, making therapeutic escape exceedingly difficult.
From a translational perspective, the research team conducted rigorous in vitro and in vivo experiments using glioblastoma cell lines and murine tumor models, observing impressive tumor growth inhibition and minimal systemic toxicity. The dual-mode cell death induction notably improved survival outcomes in preclinical models, highlighting the potential of these imidazotetrazine derivatives to elevate clinical prognosis for glioblastoma patients.
The implications of this study extend beyond mere drug development; they challenge the entrenched paradigm that temozolomide resistance is an insurmountable hurdle. By diversifying cell death pathways and addressing tumor heterogeneity, this strategy illustrates a new paradigm in cancer therapy—precision combative therapies that leverage cancer’s intrinsic metabolic liabilities and adaptive limitations.
However, while these findings are promising, several hurdles remain before clinical adoption can be realized. Comprehensive toxicity profiling, pharmacokinetics, and dose optimization must be undertaken in human trials to confirm safety and efficacy. Moreover, understanding the long-term impacts of ferroptosis induction and potential resistance mechanisms that may emerge remains critical to ensuring sustained therapeutic effectiveness.
This discovery also prompts broader inquiries into the potential for combining ferroptosis-inducing agents with existing standard-of-care treatments. The synergistic interplay of apoptosis and ferroptosis pathways could potentiate other chemotherapy agents or even immunotherapy approaches, fostering an era of combinatorial precision oncology tailored to overcomespecific resistance landscapes.
Scientifically, the elucidation of detailed molecular pathways activated by these imidazotetrazine derivatives deepens our understanding of tumor biology and chemoresistance. It highlights the intricate crosstalk between oxidative stress, iron metabolism, and apoptosis regulation within cancer cells—signaling a strategic overlap ripe for exploitation in other refractory malignancies.
The pioneering work sets a new course for addressing the intractable challenges of glioblastoma, potentially shifting clinical outcomes from dismal to hopeful. Such innovation underscores the power of chemical biology to engineer next-generation therapeutics capable of overcoming biological resilience in one of the most formidable cancer types.
As this research progresses toward clinical translation, it promises to redefine the standards of glioblastoma therapy, inspiring renewed hope among clinicians and patients alike. The ability to induce ferroptosis alongside apoptosis through single-agent therapy provides a novel, effective weapon in the ongoing war against brain cancer.
Ultimately, these findings represent a triumph of interdisciplinary science, bridging medicinal chemistry, molecular oncology, and pharmacology to surmount longstanding therapeutic barriers. If successfully developed for clinical use, these imidazotetrazine derivatives may herald a new era of durable and effective glioblastoma treatment, finally tipping the balance in favor of patient survival and improved quality of life.
Subject of Research: Novel therapeutic strategies to overcome temozolomide resistance in glioblastoma through induction of ferroptosis and apoptosis.
Article Title: Novel imidazotetrazine derivatives overcome temozolomide resistance in glioblastoma by inducing ferroptosis and apoptosis.
Article References:
Yang, H., Zhao, W., Huang, Y. et al. Novel imidazotetrazine derivatives overcome temozolomide resistance in glioblastoma by inducing ferroptosis and apoptosis. Cell Death Discov. 12, 14 (2026). https://doi.org/10.1038/s41420-025-02857-3
Image Credits: AI Generated
DOI: 10.1038/s41420-025-02857-3 (09 January 2026)
Tags: cancer resistance mechanismschemotherapeutic challenges in glioblastomadual cell death pathwaysferroptosis and apoptosisglioblastoma multiforme treatmentimproving patient survival in brain tumorsinnovative cancer drug developmentlipid peroxides and cancernew therapeutic strategies for GBMnovel imidazotetrazine drugsovercoming temozolomide resistancetargeted glioblastoma therapies