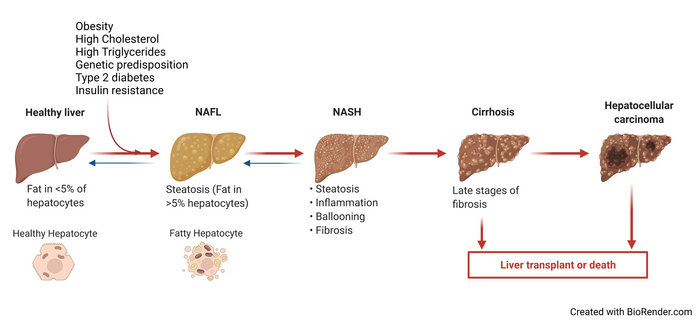
The prevalence of non-alcoholic fatty liver disease (NAFLD), one of the most widespread disorders worldwide, is expected to rise by more than 50% by 2030. Non-alcoholic fatty liver (NAFL), the initial stage of NAFLD, is associated with fat accumulation and, sometimes, mild inflammation. In some cases, NAFL can progress into a more advanced form of NAFLD, non-alcoholic steatohepatitis (NASH), resulting in significant inflammation, fibrosis, and liver damage. NASH, in turn, can advance to end-stage liver disease, cirrhosis, and hepatocellular carcinoma (HCC). Patients with NAFLD also have an increased risk of developing other types of cancers. Thus, NAFLD is clinically significant for determining the risk of cancer development, which could further help in early tumor detection and potentially improve patient outcomes.
Credit: Prof. Huiping Zhou from Virginia Commonwealth University School of Medicine, USA
The prevalence of non-alcoholic fatty liver disease (NAFLD), one of the most widespread disorders worldwide, is expected to rise by more than 50% by 2030. Non-alcoholic fatty liver (NAFL), the initial stage of NAFLD, is associated with fat accumulation and, sometimes, mild inflammation. In some cases, NAFL can progress into a more advanced form of NAFLD, non-alcoholic steatohepatitis (NASH), resulting in significant inflammation, fibrosis, and liver damage. NASH, in turn, can advance to end-stage liver disease, cirrhosis, and hepatocellular carcinoma (HCC). Patients with NAFLD also have an increased risk of developing other types of cancers. Thus, NAFLD is clinically significant for determining the risk of cancer development, which could further help in early tumor detection and potentially improve patient outcomes.
NAFLD is characterized as a metabolic disease and is mainly linked with obesity, type-2 diabetes, dysfunctional lipid metabolism, and insulin resistance. The progression of NAFLD into NASH is believed to be triggered by several factors including diet, disruption of the gut microbiota, and genetics. However, the understanding of the mechanisms that influence NAFLD development, progression, and severity is still incomplete. This has prevented the development of effective pharmacologic or biological therapeutics or diagnostic biomarkers for this disease.
Now, recent clinical studies and research on animal models have indicated that the dysregulation of bile acid and lipid (or fat) metabolism may be linked with NAFLD progression. A new Chinese Medical Journal review article highlights these findings to discuss how bile acids and sphingolipids (a specific lipid with a variety of functions) contribute to NAFLD, and how this knowledge could help treat the disease. “There is an obvious need for standardized treatment options for NAFLD. A better understanding of how bile acids and sphingolipids—which are a specific type of lipid molecule—mediate disease progression could facilitate the development of new diagnostic and therapeutic strategies for NAFLD,” explains Prof. Huiping Zhou from Virginia Commonwealth University School of Medicine, USA, who is the corresponding author of the paper.
The liver plays an important role in the fat metabolism of our body. Central to this role is the regulation of bile acids, which play a key function in digesting dietary fats and are also important signaling molecules. Bile acids regulate hepatic fat metabolism, immune responses, and the gut’s microenvironment. Any imbalance in their signaling, composition, or quantity affects the progression of NAFLD and other metabolic diseases. Clinical studies have shown that people with NAFLD exhibit elevated levels of primary bile acids in the liver, a finding closely associated with NAFLD progression, liver inflammation, NASH and fibrosis severity, and even death.
Similarly, sphingolipids are necessary structural components of the lipid membrane and essential for hepatic lipid metabolism. Ceramides and sphingosine-1-phosphate (S1P) are important sphingolipids. Like bile acids, they too play a role in signaling pathways that impact metabolic disorders, including NAFLD. Lipid profiling in animal models and human patients has shown a correlation of elevated ceramide levels with severe obesity, insulin resistance, NAFL and NASH. Diet also plays a role in causing the overexpression of mutant genes that increase ceramide levels and accelerate NASH progression. Mice models fed with a western diet and sugar water have demonstrated significant fluctuations in sphingolipid metabolism and signaling pathways. These mice models exhibited an increase in ceramide levels, steatosis, inflammation, fibrosis, and HCC. In the same way, S1P has been observed to trigger certain physiological and pathological processes, including NAFLD-linked inflammation and fibrosis.
Consequently, several studies have explored the possibility of targeting components of bile acid and sphingolipid metabolism for treating NAFLD. Bile acid sequestrants have shown promising results in preventing NASH and reversing liver damage in mice models, by reducing bile acid levels and modulating the gut microbiome and bile acid metabolism. Likewise, other animal models have demonstrated the potential of therapeutics that inhibit sphingolipid-metabolizing enzymes to moderate insulin sensitivity/resistance and hepatic steatosis. However, so far, targeted therapies focusing on bile acid pathways appear to be more practical and beneficial.
Talking about her vision for the future, Prof. Zhou says, “Future research could look into the nuanced relation between bile acids and sphingolipids, and the localization of these signaling molecules. There is also a lot of scope to understand the impact of sphingolipids on the two-way signaling between the gut and liver, gut microbiomes, and intestinal barrier function. Additionally, personalized analysis of genetic risk factors and abnormalities in bile acid circulation between the liver and intestines could hold the key to improved NAFLD diagnosis and treatment.”
Hopefully, this review would provide a roadmap for future research that would help realize her vision.
***
Reference
DOI: https://doi.org/10.1097/CM9.0000000000002156
Journal
Chinese Medical Journal
DOI
10.1097/CM9.0000000000002156
Method of Research
Systematic review
Subject of Research
Not applicable
Article Title
Bile acids and sphingolipids in non-alcoholic fatty liver disease
Article Publication Date
6-Jul-2022
COI Statement
The authors report no conflict of interest.




