A groundbreaking study published in Pediatric Research brings new hope to understanding and evaluating neonatal encephalopathy (NE), a devastating condition characterized by impaired brain function in newborns. Spearheaded by Moss, Yazdani, Jensen, and colleagues, this research harnesses the power of diffusional kurtosis imaging (DKI) to dissect white matter microstructural changes associated with injury severity and subsequent recovery. By pushing the boundaries of neuroimaging techniques, their findings promise a transformative impact on both diagnostic precision and therapeutic monitoring in this vulnerable population.
Neonatal encephalopathy is a complex syndrome that often results from hypoxic-ischemic events around the time of birth, leading to brain injury with lasting neurological consequences. Historically, assessing the extent of injury and likely outcomes has relied heavily on clinical examination and traditional magnetic resonance imaging (MRI) methods, which can sometimes be limited in sensitivity. The adoption of DKI in this arena marks a significant advancement because it can capture non-Gaussian water diffusion behavior, thereby revealing previously hidden microstructural details within brain tissue.
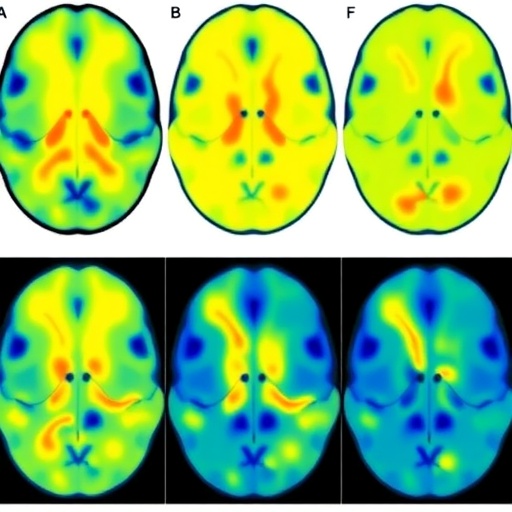
The investigators applied diffusional kurtosis imaging specifically to the white matter of neonates diagnosed with encephalopathy. This is crucial since white matter tracts are particularly susceptible to hypoxic-ischemic injury due to their high metabolic demand and developmental status during the neonatal period. DKI provides metrics such as mean kurtosis, axial kurtosis, and radial kurtosis, which correlate with tissue complexity and integrity beyond standard diffusion tensor imaging parameters. These more intricate measures allow a nuanced understanding of white matter alterations that accompany brain injury and repair processes.
By leveraging a cohort of neonates subjected to DKI scans shortly after injury and at follow-up stages, the study meticulously tracked changes in white matter microstructure that reflect injury severity. The robust imaging analysis revealed distinct kurtosis patterns that differentiate more severely affected infants from those with relatively milder impairment. This differentiation is essential for early prognostication and informed clinical decision-making, potentially guiding interventions in a timely manner to mitigate long-term disabilities.
The longitudinal aspect of this research is particularly striking. The authors demonstrated that DKI metrics evolve during the recovery phase, indicating that white matter displays dynamic reorganization and healing capabilities post-injury. Tracking these changes with high-resolution kurtosis imaging provides unprecedented insight into the brain’s resilience and plasticity in neonatal encephalopathy. Moreover, correlating imaging biomarkers with neurodevelopmental outcomes helped validate DKI’s predictive potential in real-world clinical contexts.
Such findings could revolutionize how neonatal brain injury severity is quantified. Traditional MRI methods often fail to capture subtle structural disruptions or misclassify regions of evolving injury. DKI’s sensitivity to microstructural complexity makes it an invaluable tool in delineating areas of injury that are not yet apparent morphologically, enabling earlier therapeutic interventions. This study underscores the importance of integrating advanced neuroimaging modalities into neonatal care frameworks to optimize diagnosis, prognosis, and ultimately, patient outcomes.
The implications for treatment monitoring are equally significant. Emerging neuroprotective therapies, such as therapeutic hypothermia and pharmacological agents, require rigorous assessment of efficacy in neonatal populations. The ability of diffusional kurtosis imaging to non-invasively and quantitatively monitor white matter recovery permits clinicians and researchers to evaluate treatment responses objectively, hastening the refinement of therapeutic protocols and improving individualized care pathways.
Moreover, the researchers highlight the compatibility of DKI with standard neonatal MRI protocols, which means this technique can be feasibly incorporated into existing clinical imaging workflows. This pragmatic approach is likely to accelerate adoption in neonatal intensive care units, where early and accurate brain injury assessment is critical. The translational potential of this imaging innovation could reshape current paradigms and make sophisticated neonatal brain monitoring more accessible worldwide.
Insights from this study also open new avenues for basic neuroscience research regarding white matter development and injury mechanisms. Understanding how diffusional kurtosis relates to underlying histopathological changes enriches our comprehension of neonatal brain vulnerability and repair. This could inspire future investigations aimed at identifying molecular targets for neuroprotection and regeneration during the most fragile stages of brain maturation.
Further research prompted by these findings will hopefully expand the applicability of DKI beyond neonatal encephalopathy. The technique’s sensitivity to microstructural tissue changes might prove invaluable across a spectrum of pediatric neurological disorders marked by white matter abnormalities, such as cerebral palsy or periventricular leukomalacia. This pioneering work sets the stage for harnessing advanced diffusion imaging to revolutionize brain health assessment in children.
The study’s rigorous methodology and multi-disciplinary collaboration between neuroradiologists, neonatologists, and neuroscientists contributed to a rich dataset allowing comprehensive analysis. The integration of clinical, imaging, and outcome data strengthens the validity of conclusions drawn, making a powerful case for DKI as a front-line diagnostic and monitoring tool. This represents an exemplary model for translational biomedical research where technological innovation directly meets clinical need.
Looking ahead, incorporating artificial intelligence and machine learning with DKI datasets could further enhance sensitivity and predictive capabilities. Automated image processing and pattern recognition may enable rapid, standardized assessments, reducing inter-observer variability and speeding up clinical workflows. Such integrative approaches promise a future where neonatal brain injury assessment is not only more accurate but also more efficient and accessible.
In conclusion, Moss and colleagues’ landmark study establishes diffusional kurtosis imaging as a cutting-edge method to evaluate white matter injury severity and recovery in neonatal encephalopathy. Its ability to reveal microstructural abnormalities beyond conventional imaging holds promise to improve early diagnosis, inform prognosis, and guide therapeutic interventions. This advancement stands to significantly elevate care standards for affected newborns and inspire further innovations in neonatal neuroimaging and treatment.
The impact of this research resonates beyond neonatal care, emphasizing the value of sophisticated quantitative imaging in unraveling the complexities of brain injury and repair. Such tools are key to unlocking new frontiers in understanding human neurodevelopmental disorders and enhancing long-term neurological health outcomes. With widespread adoption, diffusional kurtosis imaging may soon become a standard bearer for precision medicine in neonatal neurology, transforming lives by enabling clinicians to better see, understand, and treat early brain injury.
Subject of Research: Neonatal encephalopathy; white matter injury assessment; brain microstructure; diffusional kurtosis imaging.
Article Title: Neonatal encephalopathy: a diffusional kurtosis imaging analysis of white matter to assess injury severity and recovery.
Article References:
Moss, H.G., Yazdani, M., Jensen, J.H. et al. Neonatal encephalopathy: a diffusional kurtosis imaging analysis of white matter to assess injury severity and recovery. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04434-x
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41390-025-04434-x
Tags: advanced MRI methods for brain assessmentclinical evaluation of neonatal encephalopathydiffusional kurtosis imaging in neonatesHypoxic-ischemic injury in newbornsneonatal brain injuryneonatal encephalopathy assessmentneuroimaging techniques for brain injuryneurological consequences of neonatal injurytherapeutic monitoring in neonatestransformative impact of DKI in pediatricsunderstanding neonatal brain functionwhite matter microstructure analysis