In a groundbreaking advancement in the fight against renal cancer, researchers have uncovered a pivotal molecular mechanism by which the nuclear receptor coactivator 7 (NCOA7) exerts a suppressive effect on tumor progression. This novel insight, recently published in the journal Cell Death Discovery, elucidates how NCOA7 manipulates critical intracellular pathways to induce autophagy and reprogram lipid metabolism, subsequently inhibiting renal carcinoma growth. Central to this process is the interaction of NCOA7 with the vacuolar ATPase (V-ATPase), an enzyme complex integral to cellular homeostasis and acidification.
Renal cell carcinoma (RCC), the predominant type of kidney cancer, has long posed therapeutic challenges due to its complex biology and resistance to conventional treatments. The discovery that NCOA7 can modulate cellular processes like autophagy—often dubbed the cell’s recycling system—and lipid metabolic pathways sheds new light on prospective intervention points. Autophagy plays a dual role in cancer, sometimes fostering survival but also functioning as a mechanism for cell death under stress. By understanding how NCOA7 activates this pathway in RCC, scientists are now closer to harnessing autophagy’s tumor-suppressive potential.
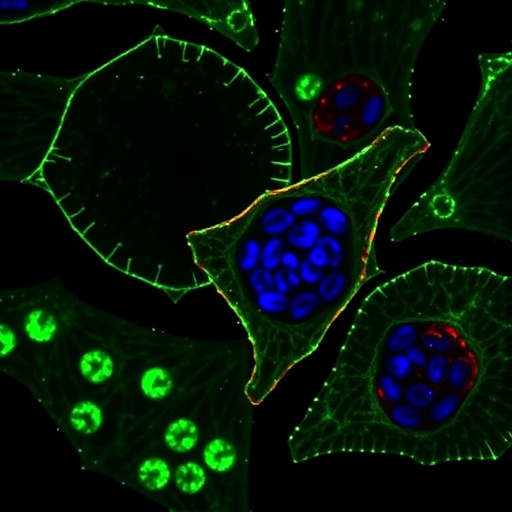
V-ATPase, the molecular target identified for NCOA7, is a proton pump essential for acidifying intracellular compartments such as lysosomes. These lysosomes are critical for degrading biomolecules and supporting autophagic flux. Interaction between NCOA7 and V-ATPase appears to optimize lysosomal function, thereby facilitating enhanced autophagic degradation. This mechanistic link not only illuminates NCOA7’s role in promoting cellular clearance but also highlights V-ATPase as a vital mediator in the suppression of renal cancer cell proliferation.
Further complicating RCC’s dysregulated environment is aberrant lipid metabolism, which cancer cells exploit for membrane synthesis and energy production. The study reveals that through its association with V-ATPase, NCOA7 orchestrates a shift in lipid metabolic pathways, likely starving tumor cells of lipid resources required for rapid division and survival. This metabolic reprogramming, coupled with increased autophagic activity, synergistically undermines tumor growth and viability.
The implications of these findings traverse beyond basic science, potentially informing the development of novel therapeutic strategies. Targeting the NCOA7-V-ATPase axis could yield compounds that specifically reactivate tumor-suppressive autophagy and disrupt pathological lipid metabolism in RCC. Moreover, the selective nature of this pathway suggests a dual benefit: diminishing tumor resilience while sparing normal cells that do not exhibit NCOA7 dysfunction.
Methodologically, the team employed an integrative approach combining molecular biology, bioinformatics, and in vivo models to validate their observations. They first demonstrated that NCOA7 expression inversely correlates with RCC progression states in patient-derived samples. Subsequent mechanistic studies deconstructed the protein-protein interaction between NCOA7 and V-ATPase and delineated downstream effects on autophagic flux and lipid enzyme expression. Animal models genetically engineered to overexpress NCOA7 displayed significant tumor regression, corroborating the clinical relevance of this pathway.
This comprehensive characterization of NCOA7’s tumor-suppressive functions not only deepens the understanding of RCC intracellular signaling but also underscores the importance of metabolic and proteostatic balance in cancer pathophysiology. It appears that the NCOA7-V-ATPase pathway functions as a molecular switch that toggles between maintaining normal cellular functions and activating cytotoxic autophagy in cancerous contexts.
From a broader perspective, this research enriches the ongoing discourse about metabolic vulnerabilities in cancer cells. Tumor-associated metabolic adaptations often provide niche survival advantages, yet they simultaneously create exploitable weaknesses. The ability to harness autophagy as an antitumor mechanism through targeting coactivators like NCOA7 represents a paradigm shift in metabolic cancer therapy.
Importantly, the therapeutic modulation of V-ATPase activity, while promising, demands caution. Given the ubiquitous role of V-ATPases in normal cellular physiology, discerning how to specifically target its cancer-associated interactions without provoking systemic toxicity is an ongoing challenge. The specificity exhibited by NCOA7’s interaction offers a blueprint for designing highly selective drugs that minimize collateral damage.
Looking forward, the study paves the way for numerous investigative pathways. It would be valuable to explore whether NCOA7 expression levels could serve as prognostic biomarkers in RCC or identify patient subsets more likely to respond to treatments modulating autophagy and lipid metabolism. Additionally, examining possible resistance mechanisms that might emerge upon pharmacological targeting of NCOA7-V-ATPase interactions is essential for clinical translation.
The integration of autophagy induction and lipid metabolic disruption exemplified by NCOA7’s function resonates with emerging cancer therapeutic strategies focusing on multi-pronged attacks on tumor survival pathways. Such approaches promise to overcome the compensation and plasticity tumors often exhibit under single-pathway therapies.
In conclusion, the meticulous elucidation of NCOA7’s inhibitory capacity on renal cancer progression through the induction of autophagy and alteration of lipid metabolism via V-ATPase interaction delivers an exciting frontier in oncology research. As scientists delve deeper into the molecular intricacies of this axis, the potential to transform RCC treatment landscapes becomes increasingly tangible. This work not only enriches molecular oncology’s knowledge base but also kindles fresh hope for patients suffering from this formidable malignancy.
The research by Wang, Luo, He, and colleagues represents a significant leap in unveiling a sophisticated network of cellular regulation instrumental in combating RCC. As the scientific community continues to unravel the complexities of cancer biology, studies like this illustrate the power of targeting intracellular machinery to reinstate the natural barriers against tumor growth.
Ultimately, the insights garnered from this compelling study advance not merely our understanding of tumor suppression mechanisms but also invigorate the quest for cutting-edge, metabolic-centric cancer therapeutics. Harnessing the full potential of the NCOA7-V-ATPase axis might well be the key to unlocking revolutionary treatments that significantly improve survival outcomes in renal cancer patients.
Subject of Research: The inhibitory role of nuclear receptor coactivator 7 (NCOA7) in renal cancer progression through regulation of autophagy and lipid metabolism via interaction with vacuolar ATPase (V-ATPase).
Article Title: NCOA7 inhibits renal cancer progression by inducing autophagy and lipid metabolism through V-ATPase interaction.
Article References:
Wang, J., Luo, H., He, Q. et al. NCOA7 inhibits renal cancer progression by inducing autophagy and lipid metabolism through V-ATPase interaction. Cell Death Discov. 11, 471 (2025). https://doi.org/10.1038/s41420-025-02766-5
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41420-025-02766-5
Tags: advancements in renal cancer researchautophagy in cancer treatmentcancer cell death mechanismsintracellular acidification and cancerlipid metabolism and renal carcinomamolecular pathways in renal cell carcinomaNCOA7 role in renal cancerrecycling systems in cancer cellsrenal cancer resistance to treatmentstherapeutic targets for renal cancertumor suppression mechanisms in RCCV-ATPase function in kidney cancer