Rheumatoid arthritis (RA) is a debilitating autoimmune disease characterized by chronic inflammation that primarily targets the synovial joints, causing pain, swelling, and eventual joint destruction. Despite significant advancements in pharmaceutical interventions, therapeutic options today merely aim to manage symptoms and retard disease progression rather than effecting a cure. A groundbreaking study published in ACS Central Science now introduces immunomodulatory nanoparticles that show promising potential in both preventing the onset of RA and mitigating the severity of disease flare-ups. This innovative approach, tested on human blood samples and animal models mimicking RA pathology, could signify a transformative leap in RA treatment paradigms.
RA pathophysiology is driven by aberrant immune responses whereby the body’s own immune system mistakenly attacks joint tissues, culminating in debilitating inflammation and cartilage erosion. Conventional disease-modifying anti-rheumatic drugs (DMARDs), such as abatacept, function by dampening immune activation but often fall short in preventing acute flare-ups or halting long-term joint damage. Notably, individuals who are seropositive for RA-related autoantibodies but asymptomatic—a condition known as pre-RA—present a therapeutic dilemma, as no approved interventions currently exist to prevent disease onset in this cohort.
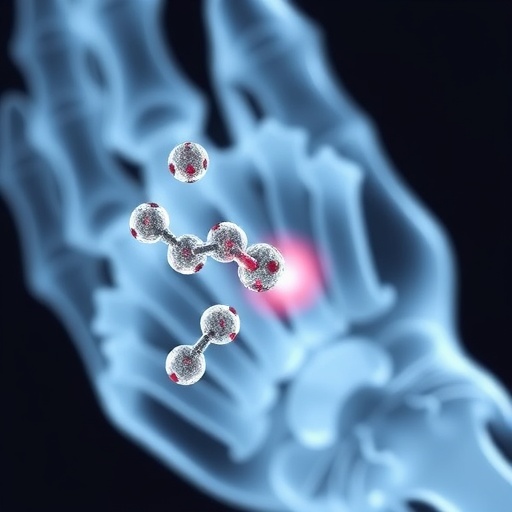
The innovative work expands upon previous research involving calcitriol-loaded nanoparticles (CLNPs), nanoscale vehicles designed to deliver calcitriol, the hormonally active form of vitamin D3, renowned for its immunoregulatory properties. The research team, led by Nisarg Shah and Nunzio Bottini, engineered these nanoparticles with additional sophistication by conjugating them with a peptide fragment derived from aggrecan (Agg), a critical extracellular matrix protein within cartilage that becomes a target of autoimmune responses in RA. This design aims to enhance the specificity of immunomodulation by selectively targeting immune cells reactive to joint-specific antigens.
.adsslot_rUN5GMDhtP{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_rUN5GMDhtP{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_rUN5GMDhtP{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
A major hurdle in nanoparticle-based therapeutics is maintaining stability and bioactivity post-manufacture. The team optimized particle size and physicochemical stability, ensuring that the nanoparticles remained contaminant-free and retained their structural integrity after being stored under freezing conditions for one month. These advances are critical for translational potential, enabling scalability and clinical applicability.
At the cellular level, dendritic cells are pivotal players in initiating and perpetuating the inflammatory cascade in RA by presenting autoantigens and activating autoreactive T cells. Experiments conducted on blood samples from both RA patients and healthy controls demonstrated that the aggrecan-conjugated CLNPs (Agg-CLNP) effectively suppressed dendritic cell activation. This downregulation of dendritic cell activity correlates with a cascading decrease in inflammatory responses, revealing the nanoparticles’ potential to modulate pathological immune activation selectively.
Animal studies utilizing a murine model of RA-like disease provided compelling in vivo evidence of the therapeutic efficacy of Agg-CLNPs. When administered prophylactically, these nanoparticles delayed the onset of symptomatic inflammation and joint swelling, underscoring their promise as a preventive strategy for at-risk populations. However, the nanoparticles exhibited limited therapeutic benefit when administered following disease establishment, highlighting the challenges of reversing established autoimmune pathology.
Intriguingly, the combination of conventional abatacept therapy with Agg-CLNPs exhibited synergistic effects, achieving more significant suppression of disease onset and progression than either treatment alone. This combinatorial approach not only reduced visible symptoms such as swelling and bone erosion but also appeared to safeguard joint integrity, underscoring the value of integrating novel nanotechnologies with existing immunomodulatory agents.
Further studies investigated the therapeutic potential of Agg-CLNPs in managing flare-ups post-corticosteroid treatment, a common clinical intervention to provide symptomatic relief in RA. Administration of the nanoparticles following corticosteroid therapy substantially diminished the frequency and severity of subsequent flares, suggesting a role for Agg-CLNPs in long-term disease management and flare prevention.
The immunomodulatory mechanism underlying these nanoparticles centers on their ability to recalibrate the immune system’s response to joint antigens without inducing broad systemic immunosuppression. By delivering calcitriol in a targeted fashion, these nanoparticles promote anti-inflammatory pathways, including modulation of dendritic cell function, skewing of T cell subsets, and suppression of pro-inflammatory cytokine secretion, collectively leading to controlled immune tolerance.
This technological advancement addresses a critical unmet need in RA therapy: the development of targeted interventions capable of both preventing disease onset in susceptible individuals and managing active disease flares with reduced systemic side effects. The nuanced design combining antigen specificity with immunoregulatory cargo establishes a blueprint for next-generation immunotherapies in autoimmune conditions beyond RA.
The study was supported by multiple funding bodies including the National Institutes of Health, Arthritis National Research Foundation, and several Swedish scientific foundations, emphasizing the multidisciplinary and international effort behind this cutting-edge research. Ethical approval was obtained through the Internal Review Board at Cedars-Sinai Medical Center, ensuring compliance with stringent standards for human and animal research.
Though preliminary, these findings herald a new era in personalized autoimmune therapeutics, where engineered nanoparticles offer precise modulation of immune responses. Continued investigations will be vital to ascertain long-term safety, dosing strategies, and potential adaptability to human patients in clinical trials. If successful, Agg-CLNPs could become a cornerstone in preventing RA progression and improving quality of life for millions affected by this challenging disease.
As RA continues to impose a significant burden on global health systems, the development of such innovative immunomodulatory platforms may pave the way for earlier intervention strategies and more effective disease control. This research not only exemplifies the power of nanotechnology in medicine but also underscores the imperative to integrate molecular insights with advanced drug delivery systems, illuminating pathways toward improved autoimmune disease management.
Subject of Research: Rheumatoid arthritis treatment using immunomodulatory nanoparticles
Article Title: Immunomodulatory Nanoparticles Enable Combination Therapies To Enhance Disease Prevention and Flare Control in Rheumatoid Arthritis
News Publication Date: 6-Aug-2025
Web References: http://dx.doi.org/10.1021/acscentsci.5c00723
Keywords: Rheumatoid arthritis, Immunomodulatory nanoparticles, Calcitriol, Aggrecan, Autoimmune disease, Disease-modifying anti-rheumatic drugs, Dendritic cells, Inflammation, Nanomedicine, Flare control, Autoimmune therapy
Tags: calcitriol-loaded nanoparticles researchchronic inflammation management in rheumatoid arthritisdisease-modifying anti-rheumatic drugs limitationsimmunomodulatory nanoparticles for autoimmune diseasesinnovative therapies for RA preventionnanoparticles for rheumatoid arthritis treatmentnew advancements in arthritis therapiespotential cures for autoimmune diseasespre-RA prevention strategiesRA pathophysiology and immune responsesrheumatoid arthritis flare management solutionstransformative approaches to joint health