Very premature babies need extra oxygen and mechanical intervention to breathe, but this damages their lungs, causing a chronic lung disease called bronchopulmonary dysplasia (BPD). These babies have smaller and weaker lungs that can’t send as much oxygen to their growing brains. The lack of oxygen during brain development can lead to learning disabilities, or problems walking, hearing and seeing.
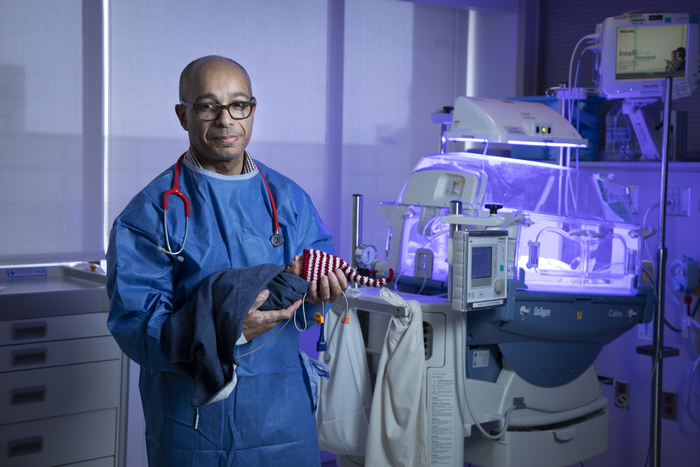
Credit: The Ottawa Hospital
Very premature babies need extra oxygen and mechanical intervention to breathe, but this damages their lungs, causing a chronic lung disease called bronchopulmonary dysplasia (BPD). These babies have smaller and weaker lungs that can’t send as much oxygen to their growing brains. The lack of oxygen during brain development can lead to learning disabilities, or problems walking, hearing and seeing.
There is no cure for BPD, but Dr. Bernard Thébaud and his team are hoping to change that. The team previously found that cells from the umbilical cord, called mesenchymal stromal cells or MSCs, could prevent BPD in newborn rats.
Now, a study in mice led by former team members Drs. Marissa Lithopoulos and Lannae Strueby and published in the American Journal of Respiratory and Critical Care Medicine shows that tiny particles released by these MSCs called extra-cellular vesicles are just as good at preventing BPD. Known as MSC-EVs or nanotherapies, these nano-sized particles have similar effects to MSCs but are easier to manufacture, store, and dose. Unlike MSCs, they can cross the blood-brain barrier, meaning they can travel into the brain after being injected into the blood stream. The researchers saw evidence that some MSC-EVs did reach the brain in this study, though most travelled to the lungs.
Not only did MSC-EVs prevent lung injury in this study, they also prevented brain injury. This was the first study to show that BPD impairs some of the key functions of brain stem cells. Brain stem cells can become all the different cells in the brain, and play an important role in brain development.
This study comes as Dr. Thébaud and his research team prepare to launch a phase I clinical trial to test the feasibility and safety of using MSCs to treat premature babies with BPD. They hope to evaluate MSC-EVs in future clinical trials.
“A therapy that improves lung and brain health would immensely benefit preterm babies with this chronic lung disease.” -Dr. Bernard Thébaud, neonatologist and senior scientist at The Ottawa Hospital and CHEO and professor at the University of Ottawa.
Full reference: Pulmonary and Neurologic Effects of Mesenchymal Stromal Cell Extracellular Vesicles in a Multifactorial Lung Injury Model. Marissa A. Lithopoulos, Lannae Strueby, Megan O’Reilly, Shumei Zhong, Marius A. Möbius, Farah Eaton, Moses Fung, Maria Hurskainen, Chanèle Cyr-Depauw, Colin Suen, Liqun Xu, Jennifer J.P. Collins, Arul Vadivel, Duncan J. Stewart, Dylan Burger, Bernard Thébaud. American Journal of Respiratory and Critical Care Medicine. https://doi.org/10.1164/rccm.202012-4520OC. Published March 14, 2022.
Core resources: Flow Cytometry and Cell Sorting Facility, High Content Imaging Core, Preclinical Imaging Core
Funding: This research was supported by the Canadian Institutes of Health Research, the Stem Cell Network, and the Ontario Institute of Regenerative Medicine, and enabled by generous donors to The Ottawa Hospital Foundation and the CHEO Foundation.
Media Contact
Amelia Buchanan
Senior Communication Specialist
Ottawa Hospital Research Institute
613-297-8315
[email protected]
Journal
American Journal of Respiratory and Critical Care Medicine
DOI
10.1164/rccm.202012-4520OC
Method of Research
Experimental study
Subject of Research
Animals
Article Title
Pulmonary and Neurologic Effects of Mesenchymal Stromal Cell Extracellular Vesicles in a Multifactorial Lung Injury Model
Article Publication Date
14-Mar-2022




