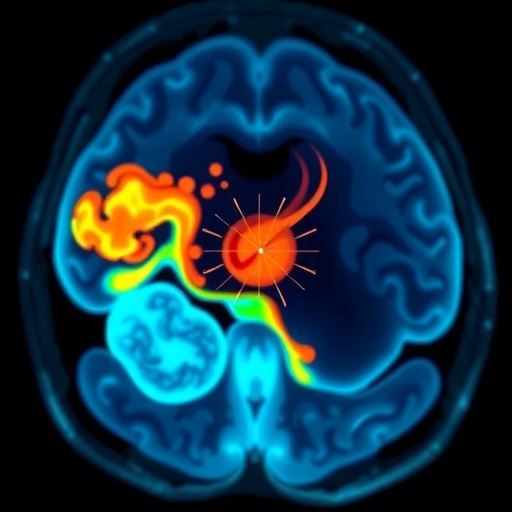
Intraventricular hemorrhage (IVH) remains a formidable challenge in the care of preterm infants, frequently complicating neonatal outcomes with severe neurological repercussions. Recent advancements in medical imaging and monitoring have prompted a groundbreaking study investigating a comprehensive, multimodal diagnostic approach to IVH by employing echocardiography, near-infrared spectroscopy (NIRS), and electrical cardiometry (EC). This innovative research, spearheaded by Hibner, Tong, Liu, and colleagues, published in the Journal of Perinatology in early 2026, sheds new light on early detection and management strategies in the fragile physiology of preterm neonates.
The complexity of IVH arises from its multifactorial etiology and subtle clinical presentation, which pose significant challenges to neonatal intensive care units globally. Traditional reliance on cranial ultrasound, while helpful, often lacks the sensitivity for real-time monitoring during the critical early phases of hemorrhage development. This necessitates the integration of additional hemodynamic and cerebral oxygenation metrics to permit proactive therapeutic intervention rather than reactive treatment.
Echocardiography stands out in this multimodal framework as a cornerstone for assessing cardiac output, structural heart anomalies, and hemodynamic stability among preterm infants at risk of IVH. The technique offers detailed visualization of cardiac anatomy alongside functional parameters, such as stroke volume and cardiac index, which are essential for understanding systemic circulatory influences that may precipitate cerebral hemorrhage. By correlating these parameters with cerebral hemodynamics, clinicians can better comprehend the pathological interplay leading to vessel rupture.
Near-infrared spectroscopy introduces a non-invasive window into cerebral oxygenation and perfusion dynamics, directly addressing the oxygen demand-supply mismatch that often accompanies IVH. NIRS technology utilizes differential absorption of near-infrared light by oxygenated and deoxygenated hemoglobin, providing continuous, bedside monitoring of regional cerebral oxygen saturation (rSO2). Such immediate feedback enables clinicians to detect early hypoxic states, facilitating prompt interventions that prevent hemorrhage progression.
Electrical cardiometry, a relatively novel approach, offers continuous, non-invasive cardiac output measurement by estimating the bioimpedance of the thoracic cavity as the heart contracts and ejects blood. This method provides dynamic insights into stroke volume and preload conditions without the need for indwelling catheters, a significant advantage in the vulnerable preterm population. Integration of EC data with echocardiographic and NIRS findings creates a comprehensive hemodynamic profile, vastly enriching understanding of cardiovascular and cerebral interrelationships in IVH.
The study meticulously enrolled preterm infants diagnosed with varying grades of IVH to ascertain the practicality and reliability of the combined diagnostic modalities. Data triangulation from these complementary techniques revealed nuanced patterns of circulatory and oxygenation changes preceding clinical deterioration. Notably, alterations in cardiac output detected via EC were often temporally aligned with fluctuations in cerebral oxygenation, underscoring a causal link warranting further exploration.
Beyond diagnostics, this multisource monitoring approach holds therapeutic implications. Precise hemodynamic data allow for individualized management of fluid status, inotropic support, and ventilatory settings, all tailored to optimal cerebral perfusion pressure. This patient-specific protocol promises to mitigate secondary brain injury and potentially improve long-term neurodevelopmental outcomes by reducing IVH severity and recurrence risk.
The authors also emphasize the practicality of implementing this multimodal monitoring in clinical settings. While echocardiography requires trained personnel and intermittent application, NIRS and EC afford continuous, bedside monitoring, ensuring real-time data availability without additional invasiveness. The synergy derived from these technologies fosters a dynamic clinical environment where neonatal care providers can make informed decisions swiftly and confidently.
Importantly, the discussion addresses potential limitations, including the sensitivity of NIRS to extracranial contamination and the influence of anatomical variability on EC signal fidelity. Ongoing technical refinements and calibration standards are advocated to enhance accuracy and reproducibility. Furthermore, expanding sample sizes and multicenter trials are encouraged to validate these findings across diverse populations and care protocols.
The investigation by Hibner and colleagues marks a paradigm shift, moving beyond single-modality assessments toward an integrated cardiovascular and neurophysiologic surveillance model. This holistic approach reflects a deeper appreciation of the interconnected nature of systemic and cerebral hemodynamics, paving the way for innovation in neonatal neurocritical care. By uniting cutting-edge technology and clinical acumen, the study sets a new benchmark for early recognition and intervention in IVH.
In the broader context of neonatal medicine, such multimodal monitoring strategies exemplify the trend toward precision medicine, where diagnostic granularity directly informs therapeutic customization. With improved early detection capabilities, healthcare teams can anticipate complications, optimize resource allocation, and possibly reduce healthcare costs by preventing downstream sequelae associated with IVH.
Future directions highlighted include integration with artificial intelligence algorithms capable of synthesizing multimodal data streams to deliver predictive analytics and decision support. Such advancements could revolutionize neonatal intensive care units by automating risk stratification and suggesting individualized interventions, all grounded in robust physiologic datasets.
Patient-centered outcomes remain the ultimate metric by which these innovations must be judged. As this multimodal technique gains traction, longitudinal studies assessing neurodevelopmental trajectories will be vital in confirming the clinical utility of refined monitoring paradigms. Early evidence is promising, but rigorous follow-up will ascertain whether the suite of technologies translates into tangible improvements in cognitive, motor, and sensory functions.
In summary, the pioneering work of Hibner et al. demonstrates a sophisticated convergence of echocardiography, near-infrared spectroscopy, and electrical cardiometry to create a potent diagnostic toolkit for intraventricular hemorrhage in preterm infants. This multimodal approach not only enhances understanding of the pathophysiology but also offers an actionable framework for early intervention. As neonatal care evolves, such integrative methodologies signal a new era of precision, responsiveness, and hope for the most vulnerable patients.
The compelling evidence presented invites widespread adoption and continued innovation, potentially transforming standards of neonatal care globally. By illuminating the invisible dynamics of neonatal circulation and cerebral oxygenation, this research empowers clinicians to confront IVH with unparalleled insight and precision. The future of preterm infant neuroprotection has never looked more promising.
Subject of Research: Multimodal diagnostic and monitoring approach for intraventricular hemorrhage in preterm infants combining echocardiography, near-infrared spectroscopy, and electrical cardiometry.
Article Title: Multimodal approach to intraventricular hemorrhage using echocardiography, near-infrared spectroscopy, and electrical cardiometry in preterm infants.
Article References:
Hibner, A.M., Tong, K., Liu, L. et al. Multimodal approach to intraventricular hemorrhage using echocardiography, near-infrared spectroscopy, and electrical cardiometry in preterm infants. J Perinatol (2026). https://doi.org/10.1038/s41372-025-02544-2
Image Credits: AI Generated
DOI: 05 January 2026
Tags: challenges in neonatal intensive carecomprehensive diagnostic approaches for IVHearly detection of neonatal brain bleedsechocardiography for IVH assessmentelectrical cardiometry applications in neonatologyhemodynamic monitoring in preterm infantsintraventricular hemorrhage in preterm infantsmultimodal monitoring of preterm brain bleedsnear-infrared spectroscopy in neonatal careneonatal imaging advancementsneurological outcomes in preterm neonatesproactive treatment strategies for IVH