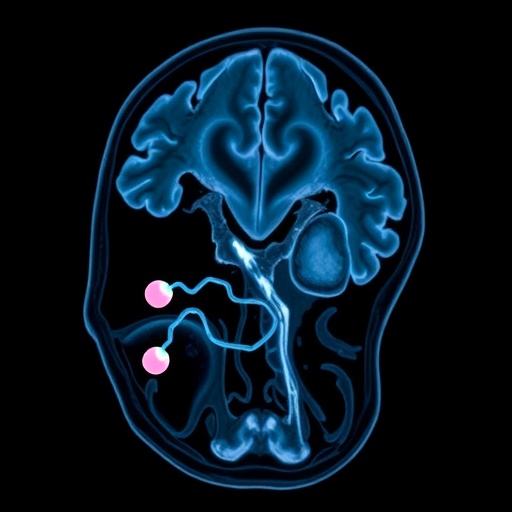
Recent advancements in neuroimaging and molecular biology have converged to uncover previously elusive connections between structural brain changes and underlying genetic mechanisms in neurodegenerative diseases. A groundbreaking study published in npj Parkinson’s Disease sheds light on multiple system atrophy (MSA), a rare and devastating neurodegenerative disorder characterized by widespread loss of neurons and glial cells. The international team behind the research, led by Chougar, Tremblay, Delva, and colleagues, utilized cutting-edge magnetic resonance imaging (MRI) techniques combined with transcriptomic analysis to demonstrate a compelling spatial alignment between MRI-detected brain atrophy patterns and the expression profiles of mitochondrial and glial genes. This novel insight deepens our understanding of MSA pathophysiology and could reshape future diagnostic and therapeutic strategies.
Multiple system atrophy is clinically heterogeneous, involving parkinsonian and cerebellar symptoms alongside autonomic failure. Despite its aggressive progression and poor prognosis, the molecular underpinnings of MSA remain incompletely understood. Previous neuropathological research has focused on abnormal accumulation of alpha-synuclein in glial cytoplasmic inclusions. However, the exact relationship between neurodegeneration and glial pathology has remained enigmatic, partly due to the lack of integrative studies correlating anatomical degeneration seen in vivo with molecular profiles at the gene expression level. This significant research gap motivated the authors to devise a multidisciplinary approach that links MRI-detected regional brain atrophy with region-specific gene expression signatures.
Employing high-resolution structural MRI data acquired from well-characterized cohorts of MSA patients, together with publicly available transcriptomic atlases derived from healthy human brain tissue, the investigators leveraged sophisticated image processing and spatial statistical models to pinpoint brain areas most affected by volume loss. These regions were then cross-referenced against the expression of genes implicated in mitochondrial function and glial cell biology—two aspects hypothesized to be central in MSA pathogenesis. Their integration of neuroimaging and transcriptomics marks a transformative step that moves the field closer to biomarker-driven precision medicine in neurodegeneration.
The results reveal pronounced atrophy within brain regions pivotal for motor control and autonomic regulation, consistent with the clinical manifestations of MSA. Remarkably, these vulnerable areas correspond spatially to regions exhibiting enriched expression of mitochondrial genes, indicating a strong link between disrupted energy metabolism and neuronal loss. Mitochondrial dysfunction has long been suspected as a contributor to neurodegenerative cascades through impaired oxidative phosphorylation, generation of reactive oxygen species, and eventual neuronal death. This study’s imaging-genomic correlation provides compelling empirical support for the mitochondrial cascade hypothesis in MSA.
In parallel, the research identifies a striking overlap between MSA-affected regions and expression patterns of glial-specific genes, particularly those involved in astrocyte and oligodendrocyte function. Glial cells, historically relegated to supportive roles, are now recognized as active participants in neuroinflammatory processes and synaptic regulation. The accumulation of alpha-synuclein within oligodendrocytes—a hallmark of MSA pathology—may exacerbate mitochondrial stress and trigger deleterious glial responses. By spatially correlating atrophy with glial gene expression, the authors propose a mechanistic link whereby glial dysfunction directly contributes to the structural neurodegeneration observed on MRI.
Interestingly, the study also delineates a gradient of involvement across different brain networks, suggesting that mitochondrial and glial gene expression patterns are not uniformly distributed but follow nuanced spatial organization that may underlie the selective vulnerability observed in MSA. This topographical specificity challenges previous assumptions of diffuse neurodegeneration and underscores the importance of regional transcriptomic diversity in shaping disease phenotypes. Such insights open avenues for targeted therapeutic interventions aimed at bolstering mitochondrial resilience and modulating glial activity within vulnerable circuits.
The methodological innovation of combining quantitative MRI metrics with spatial transcriptomics sets a new precedent for neuroscience research. By mapping imaging biomarkers onto gene expression landscapes, the study bridges the gap between macrostructural changes visible on clinical imaging and molecular pathways driving these changes. This approach not only advances knowledge in MSA but could be extrapolated to other neurological disorders where structural abnormalities and molecular dysfunction intersect, such as Parkinson’s disease, Alzheimer’s disease, and frontotemporal dementia.
From a translational perspective, the identification of mitochondrial and glial gene expression signatures as correlates of brain atrophy offers promising biomarker candidates for early diagnosis and disease monitoring. Current clinical criteria and imaging techniques often fail to distinguish MSA subtypes with sufficient sensitivity. Molecularly informed imaging protocols could enhance diagnostic precision, enabling stratification of patients for personalized therapeutic regimens. Furthermore, interventions targeting mitochondrial bioenergetics or glial cell modulation could be designed and evaluated using these spatiotemporal biomarkers as endpoints.
The study’s findings also provoke reconsideration of the role of mitochondrial health and glial function in neurodegenerative processes more broadly. They challenge the neuron-centric view by demonstrating that glial disturbances and mitochondrial impairments are intricately intertwined in driving regional brain volume loss. This integrated perspective aligns with emerging frameworks emphasizing the neurovascular unit and metabolic-immune crosstalk as critical determinants of neurodegenerative disease progression. As such, therapeutic paradigms may require reorientation towards multi-target regimens that address cellular energetics, neuroinflammation, and proteostasis collectively.
Moreover, these advances in integrative neurobiology have implications beyond therapeutics. They can refine models of disease staging by associating molecular dysfunction with anatomical decline over time. Longitudinal multimodal imaging coupled with transcriptomic profiling could track the temporal dynamics of MSA, offering prognostic information and insights into windows for intervention. This granularity enhances understanding of disease heterogeneity and augments clinical trial design by identifying molecularly defined subpopulations that may respond differently to treatment.
Despite these major contributions, the authors acknowledge several limitations needing address in future work. The dependence on transcriptomic data from neurotypical donors leaves open questions about how gene expression profiles may shift in affected individuals and across different disease stages. Moreover, the spatial resolution mismatch between imaging data and transcriptomic atlases imposes constraints on the precision of correlation analyses. Expanding these datasets to include MSA-specific postmortem gene expression and integrating other omics modalities such as proteomics and metabolomics will strengthen mechanistic understanding.
Furthermore, longitudinal clinical imaging and molecular characterization remain essential to confirm causality and temporal relationships. It is presently unclear whether mitochondrial and glial gene expression changes precede atrophy or reflect reactive adaptations. Experimental models recapitulating these molecular alterations in vulnerable cell types are also necessary to translate these insights into therapeutic advances. Nonetheless, the present study represents a pivotal first step in unveiling the molecular neuroanatomy of MSA and charts a promising course for future multidisciplinary investigations.
In conclusion, the innovative work by Chougar, Tremblay, Delva, and collaborators represents a transformative advance in neurodegenerative disease research. By unveiling a spatial concordance between MRI-derived brain atrophy and mitochondrial and glial gene expression patterns, the study provides compelling evidence for the centrality of energy metabolism and glial dysfunction in multiple system atrophy. This integrative neuroimaging and transcriptomic approach not only deepens mechanistic insight but also paves the way for molecularly informed diagnostics and targeted therapeutics. As research continues to dissect the complex interplay between cellular and structural pathology, such frameworks promise to accelerate the development of precision medicine approaches for this devastating disorder.
The convergence of advanced neuroimaging techniques with spatially resolved gene expression data heralds a new era in neuroscience, bridging scales from molecules to brain systems. This paradigm shift enables unprecedented dissection of disease mechanisms and identification of actionable targets. For multiple system atrophy, a condition urgently requiring improved clinical tools and therapies, these findings offer a beacon of hope and a template for integrative research across neurodegenerative disorders. The field eagerly anticipates further studies building on this seminal work to unravel the intricate molecular neuroanatomy that underlies brain degeneration and to harness this knowledge for patient benefit.
Subject of Research: The study investigates brain atrophy in multiple system atrophy, correlating MRI-detected structural changes with mitochondrial and glial gene expression patterns to elucidate molecular mechanisms underlying neurodegeneration.
Article Title: MRI-derived atrophy in multiple system atrophy aligns with mitochondrial and glial gene expression patterns
Article References:
Chougar, L., Tremblay, C., Delva, A. et al. MRI-derived atrophy in multiple system atrophy aligns with mitochondrial and glial gene expression patterns. npj Parkinsons Dis. (2025). https://doi.org/10.1038/s41531-025-01227-1
Image Credits: AI Generated
Tags: autonomic failure in MSAdiagnostic strategies for neurodegenerative diseasesglial gene involvement in MSAmitochondrial gene expression in neurodegenerationMRI atrophy in multiple system atrophyneurodegeneration and glial cellsneuroimaging advancements in neurodegenerative diseasesparkinsonian symptoms and glial pathologypathophysiology of multiple system atrophystructural brain changes in MSAtherapeutic approaches for multiple system atrophytranscriptomic analysis in neurodegenerative disorders