UC Irvine neurobiologists have found that genetically modified neural stem cells show positive results when transplanted into the brains of mice with the symptoms and pathology of Alzheimer’s disease. The pre-clinical trial is published in the journal Stem Cells Research and Therapy, and the approach has been shown to work in two different mouse models.
UC Irvine scientist Matthew Blurton-Jones, Ph.D.
Alzheimer’s disease, one of the most common forms of dementia, is associated with accumulation of the protein amyloid-beta in the brain in the form of plaques. While the search continues for a viable treatment, scientists are now looking into non-pharmaceutical ways to slow onset of this disease.
One option being considered is increasing the production of the enzyme neprilysin, which breaks down amyloid-beta, and shows lower activity in the brains of people with Alzheimer’s disease. Researchers from UC Irvine investigated the potential of decreasing amyloid-beta by delivering neprilysin to mice brains.
“Studies suggest that neprilysin decreases with age and may therefore influence the risk of Alzheimer’s disease,” said Mathew Blurton-Jones, an assistant professor of neurobiology & behavior. “If amyloid accumulation is the driving cause of Alzheimer’s disease, then therapies that either decrease amyloid-beta production or increase its degradation could be beneficial, especially if they are started early enough.”
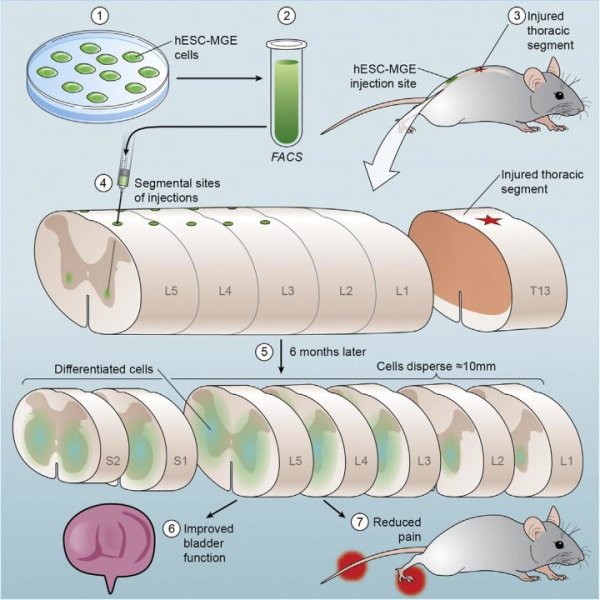
The brain is protected by a system called the blood-brain-barrier that restricts access of cells, proteins, and drugs to the brain. While the blood-brain-barrier is important for brain health, it also makes it challenging to deliver therapeutic proteins or drugs to the brain. To overcome this, the researchers hypothesized that stem cells could act as an effective delivery vehicle. To test this hypothesis the brains of two different mouse models (3xTg-AD and Thy1-APP) were injected with genetically modified neural stem cells that over-expressed neprilysin.
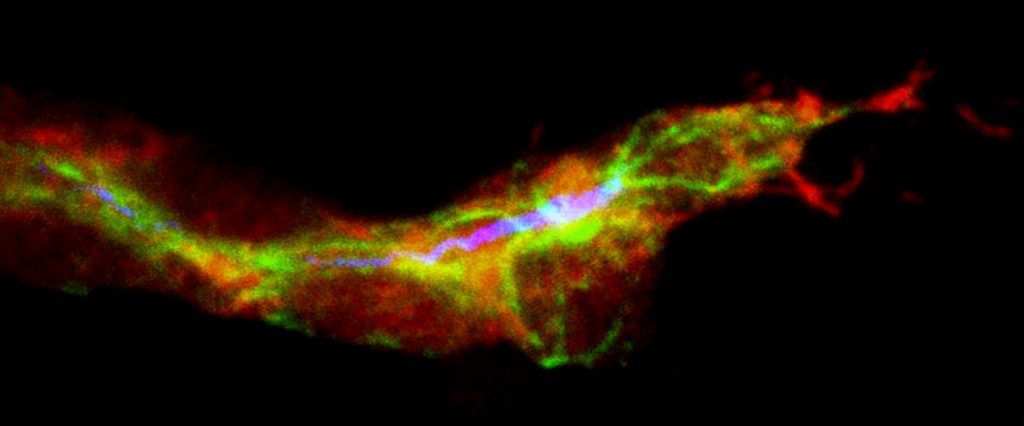
These genetically modified stem cells were found to produce 25-times more neprilysin than control neural stem cells, but were otherwise equivalent to the control cells. The genetically modified and control stem cells were then transplanted into the hippocampus or subiculum of the mice brains – two areas of the brain that are greatly affected by Alzheimer’s disease. The mice transplanted with genetically modified stem cells were found to have a significant reduction in amyloid-beta plaques within their brains compared to the controls. The effect remained even one month after stem cell transplantation. This new approach could provide a significant advantage over unmodified neural stem cells because neprilysin-expressing cells could not only promote the growth of brain connections but could also target and reduce amyloid-beta pathology.
Before this can be investigated in humans, more work needs to be done to see if this affects the accumulation of soluble forms of amyloid-beta. Further investigation is also needed to determine whether this new approach improves cognition more than the transplantation of un-modified neural stem cells.
“Every mouse model of Alzheimer’s disease is different and develops varying amounts, distribution, and types of amyloid-beta pathology,” Blurton-Jones said. “By studying the same question in two independent transgenic models, we can increase our confidence that these results are meaningful and applicable to Alzheimer’s disease. But there is clearly a great deal more research needed to determine whether this kind of approach could eventually be translated to the clinic.”
Story Source:
The above story is based on materials provided by University of California – Irvine, Shane Canning.
Article available at journal website: http://stemcellres.com/content/5/2/46