In a groundbreaking advancement that marries material science with microbiology, researchers have unveiled an innovative strategy to tackle inflammatory bowel disease (IBD) by targeting a notorious gut bacterium known as adherent-invasive Escherichia coli (AIEC). This bacteria, frequently implicated in the exacerbation of IBD, has eluded conventional treatments due to its ability to adhere intimately to intestinal cells, triggering chronic inflammation. Recent work published in Nature Communications introduces a novel approach using FimH capturing microgels, a technology designed to specifically fish out and neutralize AIEC within the complex gut environment, potentially revolutionizing therapeutic strategies for IBD patients.
Inflammatory bowel disease, encompassing Crohn’s disease and ulcerative colitis, represents a debilitating set of chronic conditions characterized by recurrent inflammation of the gastrointestinal tract. While the exact etiology of IBD remains multifactorial, a growing body of evidence places dysbiosis – the imbalance of intestinal microbial communities – as a key player in disease progression. Of particular interest is AIEC, a strain that exhibits a remarkable ability to adhere to and invade the mucosal lining of the gut, consequently provoking sustained immune responses. Targeting this bacterial strain specifically, therefore, holds the promise of interrupting this pathological cycle.
The newly engineered microgels exploit the natural adhesive properties of the AIEC bacterium. AIEC uses a fimbrial adhesin protein called FimH to latch onto mannose residues present on the surface of intestinal epithelial cells. Capitalizing on this molecular handshake, the research team developed microgels functionalized with mannose analogs that act as decoys, capturing AIEC with high specificity. These microgels function not merely as passive traps but as active agents that can sequester AIEC, preventing their attachment to the gut lining and their consequential inflammatory actions.
At the core of this technology lies a sophisticated synthesis of polymer chemistry and ligand conjugation. The microgels are composed of biocompatible hydrogel particles engineered to display dense arrays of mannose moieties on their surface. By meticulously designing the microgels’ crosslink density, size, and surface chemistry, the researchers optimized both the stability of the particles within the dynamic intestinal environment and the affinity to the FimH adhesin. This bespoke engineering ensures that the microgels remain intact in the harsh gastrointestinal milieu while maintaining avidity for AIEC.
Moving from cell culture models to animal studies, the application of FimH capturing microgels in murine models of IBD yielded compelling results. Administration of these microgels led to a marked decrease in AIEC colonization of the intestinal lining, which corresponded with attenuated inflammatory responses as measured by histopathological scoring and pro-inflammatory cytokine profiling. These preclinical data suggest that interrupting AIEC adherence can rebalance the gut microenvironment and dampen immune dysregulation associated with IBD.
Importantly, the microgel approach diverges from traditional antibiotic therapies, which broadly target microbial communities and risk inducing dysbiosis and antibiotic resistance. By honing in specifically on the pathogenic AIEC strain, this strategy minimizes collateral damage to beneficial gut microbiota, preserving microbial diversity which is critical for gut homeostasis. Moreover, the microgels, being constructed of inert and biocompatible materials, displayed minimal immunogenicity or toxicity in animal models, projecting a favorable safety profile for future human applications.
The design of these microgels also addresses a persistent challenge in gastrointestinal drug delivery: the need for materials that can navigate the complex physical and chemical environment of the gut without premature degradation. By adjusting the hydrogel matrix’s responsiveness to pH and digestive enzymes, the particles show enhanced stability through the stomach and small intestine, ensuring that they can reach the colon – a primary site of AIEC colonization and IBD inflammation – intact and functional.
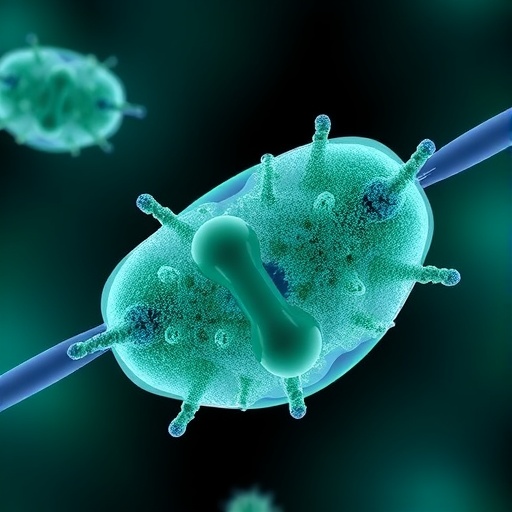
Analytical imaging techniques, including scanning electron microscopy and fluorescence microscopy, were employed to visualize the direct interactions between the FimH capturing microgels and AIEC bacteria. These images reveal densely coated bacterial surfaces wrapped in microgel particles, corroborating the biochemical assays and confirming that the particles effectively “fish out” the bacteria. This visual evidence solidifies the microgels’ proposed mechanism of action as physical interceptors in the gut lumen.
Beyond efficacy, this innovative approach may foster new avenues for patient-tailored therapies. Since IBD is heterogeneous and involves complex host-microbe interactions, interventions that can be engineered to target specific microbial factors hold promise for precision medicine in gastroenterology. By modifying ligand density or incorporating additional targeting molecules, the microgel platform could be adapted to neutralize other pathogenic bacteria or modulate microbial communities beneficially.
The study also hints at possible synergies when combining FimH capturing microgels with existing therapeutic regimens. For instance, microgels may act as adjuncts to reduce bacterial load, thereby lowering inflammation and enhancing responsiveness to immunosuppressants or biologics. This combinatorial approach may reduce the necessary dosages of systemic drugs, mitigating side effects and improving patient outcomes.
While the results thus far are promising, the pathway to clinical translation demands rigorous investigation into pharmacokinetics, long-term safety, and efficacy in diverse patient populations. Human gastrointestinal systems present additional complexities, including variabilities in microbiota composition, immune responses, and dietary factors, which may influence microgel performance. Hence, the next steps will likely involve carefully designed clinical trials to evaluate these parameters and confirm therapeutic benefits.
In the context of a broader renaissance in microbiome research, this innovation exemplifies the power of exploiting microbial molecular biology to craft highly specific interventions. The ability to selectively disarm pathogenic strains without disrupting the rich ecosystem of the gut represents a paradigm shift in managing chronic inflammatory diseases. It underscores an evolving philosophy that effective treatment strategies should be as nuanced and dynamic as the microbiota themselves.
As IBD prevalence continues to rise globally, reflected in increased healthcare burdens and patient distress, novel therapies are urgently needed. The utilization of bioengineered microgel systems tailored to intercept pathogenic bacterial adhesion introduces a new front in this battle, promising interventions that are not only effective but also sustainable and patient-friendly.
This research heralds a future where precision targeting of microbial players within the body could become commonplace, extending beyond IBD to other disorders where bacteria contribute to pathology. From urinary tract infections to periodontal diseases, pathogens leveraging surface adhesins like FimH may be caught unawares by similarly designed microgel traps, amplifying the impact of this innovative platform.
In sum, the development of FimH capturing microgels signifies a leap forward in the therapeutic manipulation of gut microbiota, offering hope for millions suffering from IBD. By ingeniously mimicking the natural ligands exploited by pathogens, these microgels serve as biological bait, intercepting harmful bacteria before they ignite destructive inflammation. As this technology evolves, it opens exciting horizons in microbiome-targeted interventions that may redefine gastrointestinal health and disease management for decades to come.
Subject of Research: Therapeutic targeting of adherent-invasive Escherichia coli (AIEC) in inflammatory bowel disease (IBD) using FimH-mannose functionalized microgels.
Article Title: Fishing out AIEC with FimH capturing microgels for inflammatory bowel disease treatment.
Article References:
Wu, J., Liu, Y., Liu, R. et al. Fishing out AIEC with FimH capturing microgels for inflammatory bowel disease treatment. Nat Commun 16, 7924 (2025). https://doi.org/10.1038/s41467-025-63276-7
Image Credits: AI Generated
Tags: adherent-invasive Escherichia coli and IBDadvancements in material science for medicinecapturing AIEC bacteria for IBD treatmentchronic inflammation and gut healthdysbiosis and its role in IBDFimH technology in microbiologyinnovative strategies for inflammatory bowel diseasemicrogels for targeted drug deliveryneutralizing gut pathogens with microgelsnovel treatment methods for ulcerative colitis.targeting gut microbiota for healththerapeutic approaches for Crohn’s disease