Microdamage in Biological Hard Tissues and Its Repair Mechanisms: Unlocking Nature’s Blueprint for Resilience
In the intricate architecture of biological hard tissues such as bone and tooth enamel, microdamage is an omnipresent phenomenon. These tissues, celebrated for their remarkable mechanical strength and resilience, are nevertheless subject to minute injuries that manifest as microcracks or diffuse damage. These microinjuries pose a complex challenge: how do these tissues endure repeated mechanical stresses throughout life, and importantly, how do they heal themselves? A recent comprehensive review published in BioMedical Engineering OnLine sheds new light on the microscopic origins of microdamage and the sophisticated biological repair mechanisms that preserve the integrity of these vital structures.
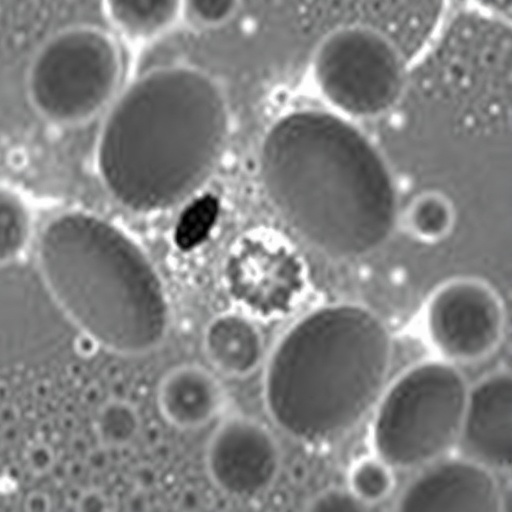
At the heart of this microdamage lies the unique, hierarchical microstructure of biological hard tissues. Unlike homogeneous synthetic materials, bone and dental tissues exhibit complex arrangements of mineral phases interwoven with organic matrices such as collagen. These intricately layered structures influence how mechanical forces are distributed and how cracks initiate and propagate. For example, the staggered alignment of mineralized collagen fibrils in bone can dissipate energy and delay crack progression, while in teeth, the enamel rods and interrod regions provide differentiated pathways that affect microcrack development. This architectural nuance is central to understanding why microdamage does not simply lead to catastrophic failure but can remain confined and even repairable.
.adsslot_otQRrgK7Du{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_otQRrgK7Du{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_otQRrgK7Du{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
Mechanical loading—ranging from everyday activities such as walking and chewing to acute trauma—drives the initiation of microdamage in hard tissues. The nature of these loads, whether tensile, compressive, or shear, alongside the frequency and duration of load application, critically affects the morphology and extent of microcracks. Additionally, macroscopic features such as bone geometry and tooth shape influence stress distribution patterns, creating hotspots where damage is more likely to accumulate. Aging introduces another layer of complexity, as alterations in material properties and regenerative capacity modify the tissue’s response to stress and propensity for microdamage.
One of the striking insights from recent research is the multifactorial influences on microdamage development. Chronic diseases such as osteoporosis and diabetes, along with pharmacological agents like bisphosphonates, affect both the formation of new microdamage and the tissue’s inherent ability to self-repair. These factors alter cellular activities, mineral metabolism, and matrix composition, which together modulate the biological response to injury. The interplay of mechanical, biological, and chemical factors thus creates a challenging environment for both diagnosis and treatment of hard tissue microdamage.
Detecting these microcracks has long posed a significant experimental challenge, given their size and the dense mineralized nature of the tissues involved. Advances in imaging technologies—such as micro-computed tomography, confocal microscopy, and nonlinear optical methods—have revolutionized the field. These tools enable researchers to non-destructively visualize microdamage in three dimensions with unprecedented resolution, capturing the spatial patterns of damage and their evolution over time. Complementing imaging are mechanical testing protocols that quantify changes in tissue stiffness, toughness, and fracture resistance, providing functional insight into the consequences of microdamage accumulation.
Understanding how hard tissues absorb and repair microdamage is a frontier area a rich with biological complexity. Bone, characterized by its dynamic remodeling cycle, utilizes a coordinated cellular response involving osteocytes, osteoclasts, and osteoblasts to identify, remove, and replace damaged matrix. Intriguingly, osteocytes sense microcracks and orchestrate targeted remodeling, a process vital for maintaining structural integrity despite ongoing microinjury. In dental tissues, repair mechanisms are less understood but involve remineralization and cellular responses in the dentin-pulp complex that can arrest crack growth or fill microdefects.
The review further highlights gaps in current knowledge—particularly regarding the molecular signaling pathways that regulate microdamage sensing and repair. While mechanical loading clearly triggers cellular events, the precise biochemical cascades remain elusive. Moreover, controversies linger about the threshold levels of damage that prompt active repair versus those that remain dormant, potentially accumulating to cause longer-term degradation. Resolving these questions requires interdisciplinary research integrating biomechanics, molecular biology, and clinical sciences.
Importantly, insights gleaned from studying microdamage in biological hard tissues have profound implications beyond biology. They inspire the burgeoning field of biomimetic materials, which seeks to replicate nature’s balance of strength and self-healing in synthetic constructs. By decoding the structural features and repair strategies of bone and tooth enamel, engineers can design novel materials that better resist fatigue, self-repair minor damage, and extend longevity—promising breakthroughs for implants, prosthetics, and structural materials.
Furthermore, the ability to predict and control microdamage development opens new avenues for preventive and therapeutic interventions in medicine. For instance, personalized assessments of bone quality beyond mere density measures may better predict fracture risk. Similarly, targeted drug delivery or mechanical conditioning protocols could enhance the natural repair capacity of hard tissues, mitigating the debilitating effects of aging and disease.
From a clinical perspective, this review underscores the necessity for advanced diagnostic tools to detect early microdamage before it manifests as overt fractures or tooth cracks. It argues for the integration of imaging technologies with biomechanical modeling and biological assays to provide a multidimensional picture of tissue health. This multidisciplinary approach will pave the way for more effective interventions and improved patient outcomes.
The path forward in this field is both exciting and challenging. Future research directions proposed by the authors include in vivo monitoring of microdamage and repair dynamics, elucidation of molecular regulators and signaling networks, and the exploration of genetic factors influencing individual susceptibility to damage. Additionally, the development of sophisticated in vitro models that mimic physiological loading and biological environments will accelerate mechanistic studies and biomaterial innovations.
Equally compelling is the role of aging and systemic conditions on microdamage behavior. Understanding how these extrinsic factors modulate repair processes holds promise for combating degenerative diseases. For example, unraveling how diabetic conditions weaken the bone’s repair machinery may inspire novel therapies targeting metabolic pathways alongside conventional mechanical interventions.
Finally, this comprehensive analysis reveals the critical importance of viewing biological hard tissues not as passive load bearers but as dynamic, self-regulating systems continuously balancing damage and repair. This perspective not only enriches our understanding of tissue biomechanics but also redefines clinical and engineering strategies aimed at preserving or enhancing tissue function throughout the human lifespan.
In sum, the study of microdamage and its repair mechanisms in biological hard tissues represents a vital intersection of biomechanics, cell biology, and materials science. As researchers unravel the nuanced interplay between microstructure, mechanics, and biology, they edge closer to unlocking nature’s blueprint for resilience—a blueprint ripe for translation into groundbreaking medical and engineering solutions that could transform human health and material performance worldwide.
Subject of Research: Microdamage occurrence and repair mechanisms in biological hard tissues including bone and teeth.
Article Title: Microdamage in biological hard tissues and its repair mechanisms
Article References: Cao, X., Xiao, S., Shen, C. et al. Microdamage in biological hard tissues and its repair mechanisms. BioMed Eng OnLine 24, 102 (2025). https://doi.org/10.1186/s12938-025-01423-3
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s12938-025-01423-3
Keywords: Biological hard tissues, microdamage, microcracks, bone remodeling, tooth enamel, damage repair, biomechanics, imaging technologies, biomimetic materials
Tags: biological repair processesBioMedical Engineering OnLine reviewcollagen in biological tissuesenamel rod structure and functionenergy dissipation in bonehierarchical microstructure of bonemechanical strength of bone and enamelmicrocracks in dental structuresmicrodamage in biological hard tissuesmicroinjuries in hard tissuesrepair mechanisms in bone and teethresilience of biological hard tissues