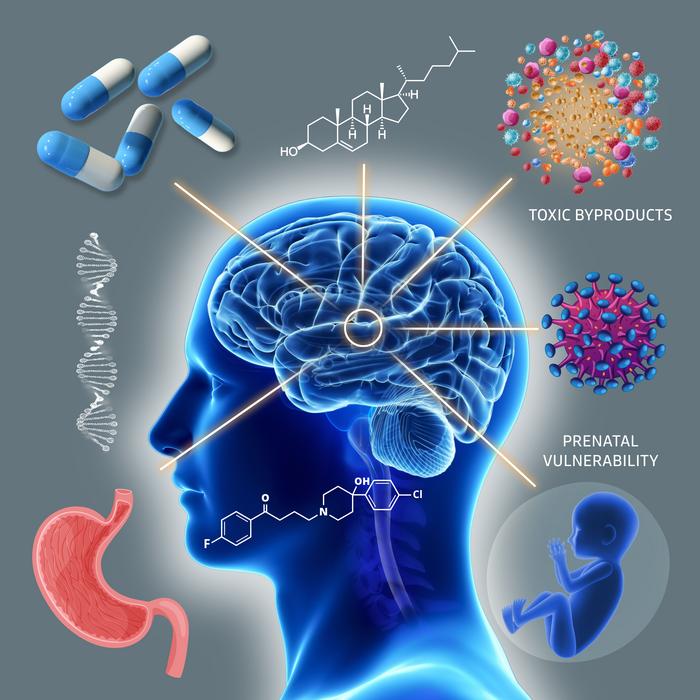
A recent editorial published in Brain Medicine has sparked significant concern regarding the potential risks posed to brain development by a class of widely prescribed medications. Authored by Editor-in-chief Julio Licinio, the piece brings to light the troubling implications of medication-induced disruption of sterol biosynthesis, highlighting the urgent need for reassessment in drug safety evaluations. This disruption is notably attributed to various FDA-approved drugs that inhibit DHCR7, a critical enzyme in cholesterol synthesis. These compounds, which include psychiatric medications like aripiprazole, trazodone, haloperidol, and cariprazine, alter cholesterol levels and ultimately impact brain functionality in ways that have primarily gone unregulated.
Dr. Licinio emphasizes that the inhibition of the DHCR7 enzyme leads to elevated levels of 7-dehydrocholesterol (7-DHC) in the body, which is not just a benign side effect. The editorial discusses how these changes invoke a biochemical profile reminiscent of certain congenital metabolic disorders, implicating a connection between routine medication and potential neurodevelopmental disruptions. Through rigorous empirical validation across various models, the disturbing nature of this association is illuminated, suggesting a re-evaluation of the frameworks within which these medications are assessed prior to public approval.
One of the core arguments presented is that these medication-induced alterations become particularly critical during vulnerable life stages, such as pregnancy. The editorial argues that current drug safety evaluations inadequately account for the combined effects of these agents, particularly in polypharmacy situations where multiple medications might be prescribed concurrently. The potential for synergistic toxicity arises, which could cause levels of toxic metabolites to surge, magnifying the risks for unsuspecting patients.
Furthermore, Dr. Licinio notes that approximately 1-3% of the population carries single-allele DHCR7 mutations, which heighten their susceptibility to adverse effects resulting from medications. For these individuals, even a single prescription could destabilize their biochemical balance, creating a state similar to Smith-Lemli-Opitz Syndrome, a severe developmental disorder characterized by significant neurological impairment. This fact underlines the critical need for genetic awareness in prescribing practices, as certain patient populations may inadvertently face grave risks due to overlooked genetic predispositions.
The alarming specifics of these pharmaceutical interactions and their potential neurotoxic outcomes are underscored by Dr. Licinio’s assertion that the implications of expansive prescription practices could result in serious long-term consequences for brain health. The editorial suggests that a multi-faceted strategy be adopted, encompassing both the reduction of medication complexity in vulnerable groups and promoting focused genetic testing. It is posited that immediate steps should be taken to safeguard populations that are most at risk, particularly expectant mothers who may unknowingly expose their developing children to hazardous compounds.
Another pivotal assertion made in the editorial pertains to regulatory processes and their current inadequacies. Dr. Licinio calls for critical reforms in drug approval processes, advocating for mandatory sterol biosynthesis screenings for agents that impact brain development. The appeal highlights the necessity to reflect real-world prescribing patterns rather than continuing to rely on static and insular testing methodologies. This call to action urges both the medical community and regulatory bodies to adapt and ensure that patient safety is prioritized.
In addressing the implications for clinical practice, Dr. Licinio outlines specific recommendations targeting vulnerable populations. Pregnant women, especially those identified with the DHCR7 mutation, should be counseled against the use of medications known to elevate 7-DHC levels. Additionally, a proactive approach involving genetic testing for women of childbearing age who are prescribed such medications could help mitigate risks. Furthermore, avoiding polypharmacy involving drugs that disrupt sterol synthesis is emphasized as a critical preventive measure to safeguard the health of both mother and child.
By shedding light on the intersection between pharmacology and neurodevelopment, the editorial serves as a profound reminder of the complexities involved in medication management. It compels healthcare professionals to reevaluate their prescribing habits, ensuring they remain cognizant of the broader biochemical impacts their choices may have on vulnerable populations. The ramifications of such discussions extend beyond just individual health; it encompasses the collective responsibility shared by the medical community in light of public health concerns tied to developmental neurobiology.
In summation, the editorial in Brain Medicine shines a crucial spotlight on an issue that has largely remained in the shadows and unacknowledged within the broader context of medicine. As awareness grows around the potential hazards of medication-induced sterol disruption, a stronger dialogue around drug safety, genetics, and regulatory practices must be fostered. Dr. Licinio’s text is more than a mere cautionary tale; it is a call for concerted action among clinicians, patients, and regulators to proactively address and reframe the norms surrounding pharmaceutical intervention in sensitive populations.
The content denotes a dramatic shift towards recognizing the intricate relationship between medications and brain health, compelling the scientific community to reframe traditional paradigms of drug testing and patient safety. Now more than ever, the urgent need for a collaborative approach in research, regulation, and clinical practice is paramount as we endeavor to safeguard future generations from the potentially deleterious effects of prescribed interventions.
Subject of Research:
Article Title: Medication-induced sterol disruption: An overlooked threat to brain development and public health
News Publication Date: 22-Apr-2025
Web References:
References:
Image Credits: Julio Licinio
Keywords
Tags: 7-dehydrocholesterol effectsbrain development riskscholesterol synthesis inhibitorscongenital metabolic disorders associationDHCR7 enzyme impactdrug safety evaluationsempirical validation of medication risksMedication-induced sterol disruptionneurodevelopmental disorders connectionpsychiatric medications side effectspublic health implicationsreassessment of FDA-approved drugs.