New AI strategies automate assessments of stored blood, remove human subjectivity
Credit: Minh Doan, Joseph Sebastian, Tracey Turner, Jason Acker, Michael Kolios, Anne Carpenter
Each year, nearly 120 million units* of donated blood flow from donor veins into storage bags at collection centres around the world. The fluid is packed, processed and reserved for later use. But once outside the body, stored red blood cells (RBCs) undergo continuous deterioration. By day 42 in most countries, the products are no longer usable.
For years, labs have used expert microscopic examinations to assess the quality of stored blood. How viable is a unit by day 24? How about day 37? Depending on what technicians’ eyes perceive, answers may vary. This manual process is laborious, complex and subjective.
Now, after three years of research, a study published in the Proceedings of the National Academy of Sciences unveils two new strategies to automate the process and achieve objective RBC quality scoring — with results that match and even surpass expert assessment.
The methodologies showcase the potential in combining artificial intelligence with state-of-the-art imaging to solve a longstanding biomedical problem. If standardized, it could ensure more consistent, accurate assessments, with increased efficiency and better patient outcomes.
Trained machines match expert human assessment
The interdisciplinary collaboration spanned five countries, twelve institutions and nineteen authors, including universities, research institutes, and blood collection centres in Canada, USA, Switzerland, Germany and the UK. The research was led by computational biologist Anne Carpenter of the Broad Institute of Harvard and MIT, physicist Michael Kolios of Ryerson University’s Department of Physics, and Jason Acker of the Canadian Blood Services.
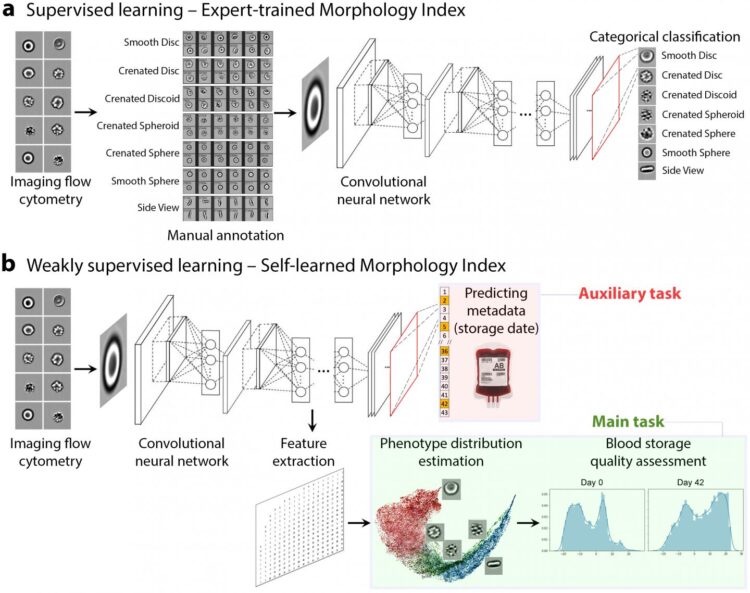
They first investigated whether a neural network could be taught to “see” in images of RBCs the same six categories of cell degradation as human experts could. To generate the vast quantity of images required, imaging flow cytometry played a crucial role. Joseph Sebastian, co-author and Ryerson undergraduate then working under Kolios, explains.
“With this technique, RBCs are suspended and flowed through the cytometer, an instrument that takes thousands of images of individual blood cells per second. We can then examine each RBC without handling or inadvertently damaging them, which sometimes happens during microscopic examinations.”
The researchers used 40,900 cell images to train the neural networks on classifying RBCs into the six categories — in a collection that is now the world’s largest, freely available database of RBCs individually annotated with the various categories of deterioration.
When tested, the machine learning algorithm achieved 77% agreement with human experts. Although a 23% error rate might sound high, perfectly matching an expert’s judgment in this test is impossible: even human experts agree only 83% of the time. Thus, this fully-supervised machine learning model could be effective to replace tedious visual examination by humans with little loss of accuracy.
Even so, the team wondered: could a different strategy push the upper limits of accuracy further?
Machines surpass human vision, detect cellular subtleties
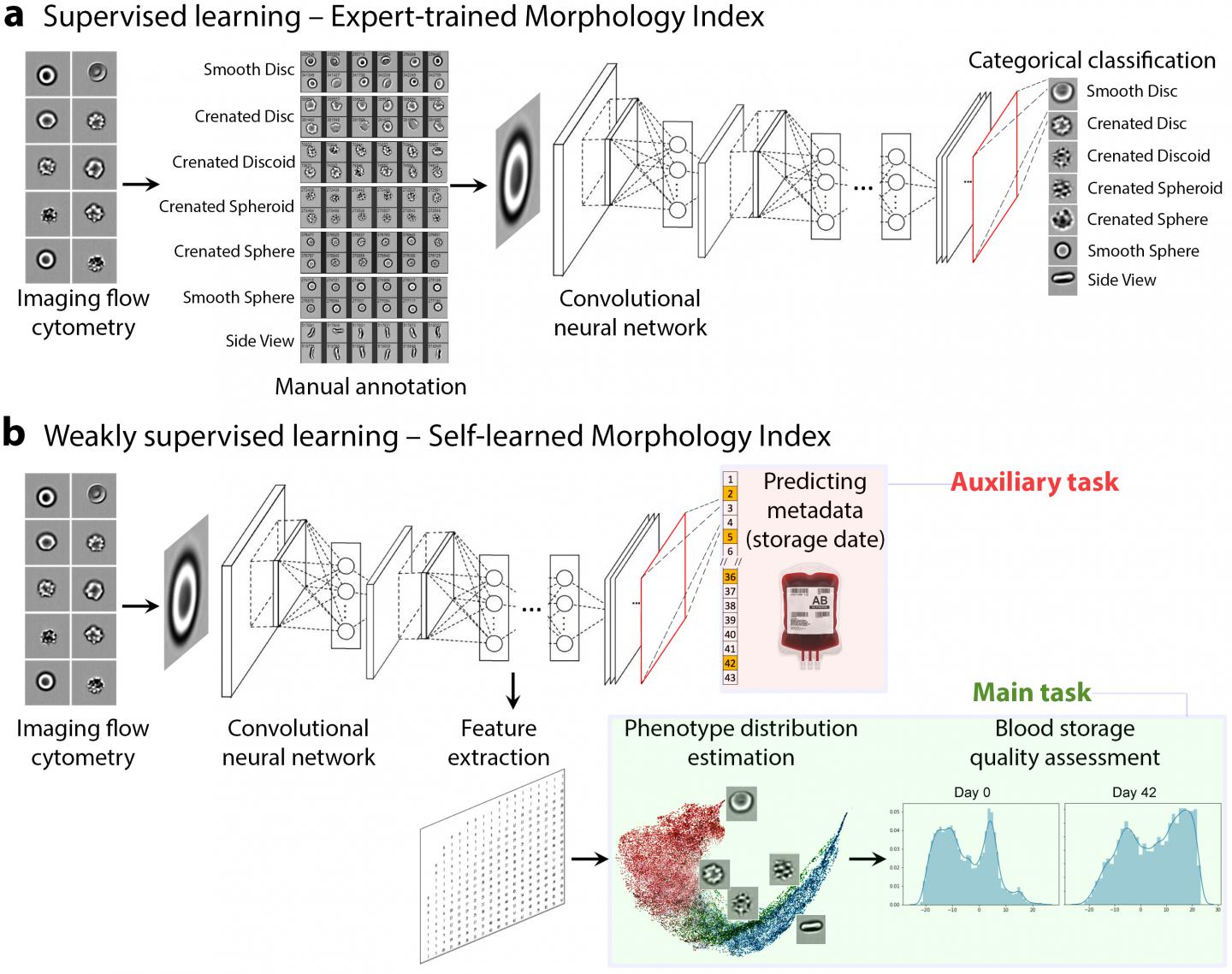
In the study’s second part, the researchers avoided human input altogether and devised an alternative, “weakly-supervised” deep learning model in which neural networks learned about RBC degradation on their own.
Instead of being taught the six visual categories used by experts, the machines learned solely by analyzing over one million images of RBCs, unclassed and ordered only by blood storage duration time. Eventually, the machines correctly discerned features in single RBCs that correspond to the descent from healthy to unhealthy cells.
“Allowing the computer to teach itself the progression of stored red blood cells as they degrade is a really exciting development,” says Carpenter, “particularly because it can capture more subtle changes in cells that humans don’t recognize.”
When tested against other relevant tests such as a biochemical assay, the weakly-supervised trained machines predicted RBC quality better than the current six-category assessment method used by experts.
Deep learning strategies: Blood quality and beyond
Further training is still needed before the model is ready for clinical testing, but the outlook is promising. The fully-supervised machine learning model could soon automate and streamline the current manual method, minimizing sample handling, discrepancies and procedural errors in blood quality assessments.
The second, alternative weakly-supervised framework may further eliminate human subjectivity from the process. Objective, accurate blood quality predictions would allow doctors to better personalize blood products to patients. Beyond stored blood, the time-based deep learning strategy may be transferable to other applications involving chronological progression, such as the spread of cancer.
“People used to ask what the alternative is to the manual process,” says Kolios. “Now, we’ve developed an approach that integrates cutting-edge developments from several disciplines, including computational biology, transfusion medicine, and medical physics. It’s a testament to how technology and science are now interconnecting to solve today’s biomedical problems.”
###
*Data reported by the World Health Organization
Funding: US National Science Foundation / UK Biotechnology and Biological Sciences Research Council joint grant (awarded to AEC and PR), a Biotechnology and Biological Sciences Research Council grant (awarded to PR), the Natural Sciences and Engineering Research Council of Canada (NSERC) and the Canadian Institutes of Health Research (CIHR) via a Collaborative Health Research Projects (CHRP) grant (awarded to MCK and JPA), a grant administered by Carigest S.A. of Geneva, Switzerland (to AR), funding from the federal (Health Canada) and Provincial and Territorial Ministries of Health for The Canadian Blood Services research program. Experiments were performed at the University of Alberta Faculty of Medicine & Dentistry Flow Cytometry Facility, which receives financial support from the Faculty of Medicine & Dentistry and Canada Foundation for Innovation (CFI) awarded to contributing investigators.
Media Contact
Suzana Pinto
[email protected]
Original Source
https:/
Related Journal Article
http://dx.