Low-tech – just what the doctor ordered
Credit: University of Leeds/Dr Pete Culmer
Low-tech – just what the doctor ordered
Medical equipment that can be manufactured at low cost, is simple to use and can be easily maintained will help extend surgery to the 5 billion people worldwide who currently cannot get access to it, say researchers.
Writing in the IEEE Journal of Translational Engineering in Health and Medicine, they argue that surgical technology is often developed for well-resourced healthcare systems – and is of little or no use in poorer settings where hospitals lack sophisticated support infrastructure or appropriately trained staff.
Without access to medical equipment they can use, hospitals and clinics in low-to-middle income countries cannot offer surgical treatment to nine out of ten patients.
An international research team led by the University of Leeds is calling for a focus on creating medical devices specifically for use in low-to-middle income countries. They have pioneered a development approach based on “participatory design”, where the users of the technology are closely involved in its design – and where functionality of the device is pared back to key essentials.
To demonstrate their approach, the researchers describe how they designed a simplified surgical tool for performing laparoscopic – or keyhole surgery – in low resource settings. The result is that laparoscopic surgery can now be carried out in clinics and hospitals where it was not possible before.
Dr Pete Culmer, Associate Professor in Healthcare Technologies at Leeds, who supervised the research, said: “Laparoscopic surgery has benefits for patients. People recover more quickly, and the risks of cross infection are lower.
“But in many parts of the world, laparoscopic techniques are not widely used because of the need to use equipment that cannot be easily maintained or relies on complex infrastructure in the operating theatre.
“We partnered with clinicians in India to work on developing instruments that would make the process simpler, with the aim of enabling laparoscopic surgery to be available in more locations around the world.”
Access to safe surgery
During laparoscopic operations, the surgeon inflates the patient’s abdomen with CO2 gas, to create space to see internal organs and to manipulate instruments. That comes with two challenges. It requires operating theatres to have a reliable CO2 gas supply. It also requires the patient’s abdominal muscles to be fully relaxed requiring a general anaesthetic and an anaesthetist to give it.
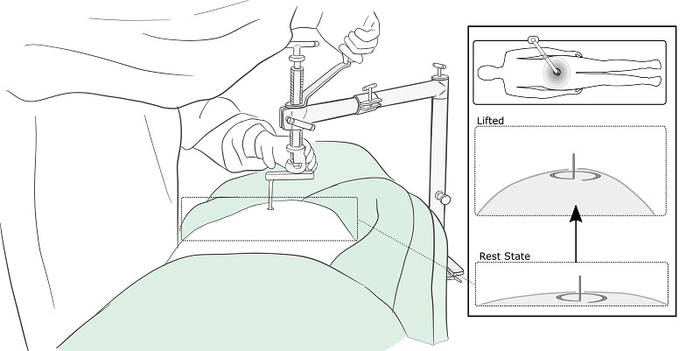
An alternative approach called gasless laparoscopy has been developed. Rather than pumping CO2 into the abdomen, a mechanical retractor or clamp is used to lift the abdominal wall. With this method, the patient does not need a general anaesthetic – instead, a spinal anaesthesia is given, and there is no need for a dedicated anaesthetist to be present.
But this alternative approach has failed to gain popularity, largely because of challenges with using and maintaining the retractors.
Fit for purpose
The researchers, in partnership with surgeons and a medical device manufacturer in India, designed a new retractor, ensuring it was fit for purpose in a low-resourced healthcare setting.
The attached graphic shows how a small ring is manipulated onto the end of the retractor by a surgeon using keyhole techniques. When in place, the device is manually operated to gently lift the abdominal cavity upwards, creating the necessary space for the surgical team to operate.
Known as RAIS (Retractor for Abdominal Insufflation-less Surgery), the innovative retractor went through five design iterations before a prototype was developed and tested.
During a clinical evaluation, it was used in 12 laparoscopic operations: in four cases of appendicitis, two hysterectomies and six cases where the gall bladder was removed.
The scientific paper reports that there were no adverse events from using the retractor.
Dr Jesudian Gnanaraj, a surgeon who has pioneered gasless laparoscopic surgery and worked extensively in parts of rural India where surgery has not typically been available, said: “The biggest problem for rural surgeons needing to provide laparoscopic surgery is finding an anaesthesiologist and the equipment to give general anaesthesia.
“The RAIS device makes laparoscopic surgery possible, with lower costs and easily available resources like spinal anaesthesia.
“Providing laparoscopic surgery can help rural patients get back to work as soon as possible. This is vital because the longer they take to recover, the higher the chance of them falling below the poverty line.”
Writing in the research paper, the researchers said the device was “…considered convenient to setup in the operating theatre, could be readily cleaned and sterilised and transported within and between rural surgical sites”.
The simplified design of the retractor meant it was easier for the device manufacturer to get regulatory approval, with the time it takes to go from design to approval being four years in this case. It can sometimes take ten years.
The RAIS device meets the guidelines established by the World Health Organisation for the design and development of healthcare technology for low to middle income countries. It says they should follow four key principles, the 4As – affordability, accessibility, availability and appropriateness.
END
Note to editors
The paper – The RAIS device for global surgery: using a Participatory Design approach to navigate the translational pathway to clinical use – can be downloaded from IEEE Explore.
For further details and for requests to talk to Dr Pete Culmer, please contact the press office at the University of Leeds: [email protected]
Research collaboration
The research team included:
-
Association of Rural Surgeons of India and International Federation of Rural Surgeons, Biru, India: Gnanaraj Jesudian.
-
Maulana Azad Medical College, New Delhi, India: Anurag Mishra, Department of Surgery, Lovenish Bains, Department of Surgery.
-
Ortho Life Systems, New Delhi, India: Sundeep Singh Sawhney, Tamandeep Singh Kochhar.
-
Pd-m International Ltd, Thirsk, UK: Philippa Bridges, Richard Hall.
-
University of Leeds, UK: Noel Aruparayil, Leeds Institute of Medical Research at St. James’s Hospital; Cheryl Harris, Leeds Institute of Medical Research at St. James’s Hospital; Peter Culmer, School of Mechanical Engineering; Millie Marriott Webb, School of Mechanical Engineering.
END
DOI
10.1109/JTEHM.2022.3177313
Method of Research
Randomized controlled/clinical trial
Subject of Research
People
Article Title
The RAIS device for global surgery: using a Participatory Design approach to navigate the translational pathway to clinical use
Article Publication Date
23-May-2022




