In a groundbreaking advance amidst the challenges of neonatal intensive care, recent research reveals that reduced heart rate variability (HRV) may serve as a crucial predictive biomarker for severe intraventricular hemorrhage (sIVH) in extremely preterm infants. The findings, detailed in a study led by Smolkova et al., highlight the nuanced interplay between autonomic nervous system regulation and the vulnerability of the preterm brain, offering fresh insights into early diagnostics that could reshape clinical approaches to one of the most devastating complications of extreme prematurity.
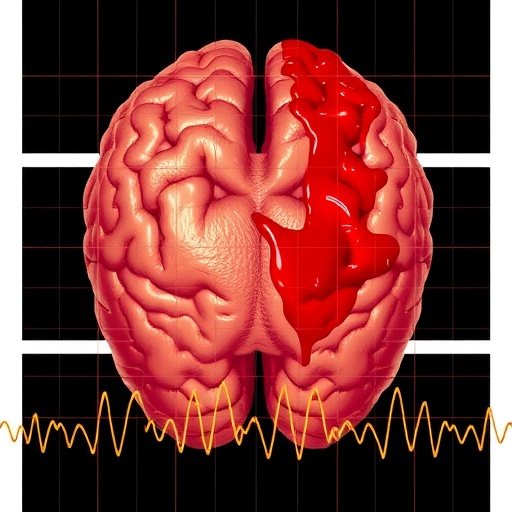
Intraventricular hemorrhage is a severe neurological complication commonly seen in infants born before 28 weeks of gestation, resulting from the fragility of the germinal matrix vasculature. The hemorrhage often leads to devastating outcomes, including long-term neurodevelopmental impairment and even mortality. Despite advances in neonatal care, early identification of infants at greatest risk remains a critical challenge. This new study explores heart rate variability metrics, a window into autonomic nervous system function, as a non-invasive prognostic tool for sIVH.
Heart rate variability, the natural fluctuation in beat-to-beat intervals of the heart, reflects the dynamic balance between sympathetic and parasympathetic nervous systems. In healthy neonates, a robust HRV indicates adaptive autonomic responses and stable cardiovascular control. However, diminished HRV suggests autonomic dysregulation, which can correlate with systemic instability or underlying neuropathology. Prior research identified links between low HRV and poor outcomes in preterm infants, but the specificity of various HRV metrics in predicting severe intraventricular hemorrhage had remained elusive until now.
The study systematically analyzed continuous electrocardiogram recordings from a cohort of extremely preterm infants, tracking HRV metrics within the crucial first weeks of life. Utilizing advanced time-domain and frequency-domain analyses, researchers pinpointed which parameters most reliably signaled an impending severe hemorrhagic event. Their novel approach integrated HRV indices with clinical variables, creating a predictive model with promising sensitivity and specificity.
Findings indicated that diminished low-frequency (LF) power and reduced root mean square of successive differences (RMSSD) were particularly predictive of sIVH onset. The LF component of HRV is believed to reflect baroreflex activity and sympathetic modulation, while RMSSD predominantly captures parasympathetic tone. The concurrent reduction in these metrics suggests a profound autonomic imbalance precedes the clinical manifestations of severe hemorrhagic injury to the brain.
Importantly, the temporal evolution of HRV changes also provided diagnostic clues. Infants who subsequently developed sIVH demonstrated an early, sustained suppression of HRV within the first 72 hours post-birth, preceding radiological confirmation of hemorrhage by days in some cases. This latency underscores HRV’s potential as an early physiological marker before irreversible brain injury manifests on imaging, allowing for timely intervention strategies.
Clinicians currently lack reliable bedside monitoring tools to predict imminent sIVH, relying mostly on periodic cranial ultrasounds that may lag behind evolving pathology. Incorporating real-time HRV analysis into neonatal intensive care units could transform monitoring paradigms, enabling continuous risk assessment and potentially guiding modified supportive treatments aimed at stabilizing autonomic function and cerebral blood flow.
The implications of this research extend beyond prognosis to possibly influencing therapeutic avenues. Autonomic regulation plays a critical role in cerebral perfusion stability, and interventions that bolster parasympathetic activity or modulate sympathetic overdrive might mitigate the risk of vessel rupture within the germinal matrix. Emerging modalities such as vagal nerve stimulation or pharmacologic agents targeting autonomic pathways could be evaluated based on HRV readouts as surrogate endpoints.
However, translating these findings into routine clinical practice requires further validation in larger, multi-center cohorts, spanning diverse neonatal care settings. Variability in monitoring equipment, signal processing algorithms, and infant comorbidities poses challenges that must be addressed to standardize HRV measurement protocols and validate predictive cutoffs. Prospective studies assessing HRV-guided interventions will be pivotal in determining whether early detection truly alters clinical outcomes.
Additionally, integrating HRV with other biomarkers—biochemical, neuroimaging, or genetic—could refine risk stratification models, providing a multidimensional approach to identifying infants at highest probability of severe IVH. Combining these data streams may unveil complex pathophysiological mechanisms underpinning hemorrhage, fostering a holistic understanding that bridges cardiovascular, neurological, and developmental domains.
Beyond its immediate application to intraventricular hemorrhage, the study exemplifies the burgeoning field of neonatal neurocardiology, where cardiac autonomic signals are leveraged to decipher vulnerability in the developing brain. The research advances the paradigm that systemic physiological signals beyond traditional vital signs harbor untapped prognostic information, encouraging innovation in sensor technology and analytic methodologies applicable across critical care.
The profound challenge of caring for extremely preterm infants mandates precise, non-invasive tools to anticipate complications early and personalize interventions. This study’s identification of HRV as a key predictive marker for sIVH could revolutionize neonatal monitoring, potentially reducing the incidence and severity of hemorrhagic brain injury with profound implications for lifelong neurodevelopmental outcomes.
In conclusion, the work by Smolkova and colleagues charts an exciting path forward, portraying heart rate variability not merely as a physiological curiosity, but as a pivotal clinical biomarker in neonatal intensive care. The compelling evidence positions HRV metrics, especially LF power and RMSSD, at the forefront of efforts to predict and ultimately prevent severe intraventricular hemorrhage in the most vulnerable patients. Continued research and clinical integration of these findings hold promise for improving survival and quality of life for countless preterm infants worldwide.
Subject of Research: The predictive value of heart rate variability (HRV) metrics for severe intraventricular hemorrhage (sIVH) in extremely preterm infants.
Article Title: Reduced heart rate variability predicts severe intraventricular haemorrhage in extremely preterm infants
Article References:
Smolkova, M., Sunwoo, J., Kim, S.H. et al. Reduced heart rate variability predicts severe intraventricular haemorrhage in extremely preterm infants. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04632-7
Image Credits: AI Generated
DOI: 01 December 2025
Tags: autonomic nervous system regulationchallenges in neonatal careclinical approaches to brain bleedsearly diagnostics for sIVHheart rate variability metricslow heart rate variabilityneonatal intensive care advancementsneurodevelopmental impairment in infantsnon-invasive prognostic toolsoutcomes of extreme prematuritypredictive biomarker for preterm infantssevere intraventricular hemorrhage