Recent advancements in the field of reproductive health have illuminated the intricate relationship between polycystic ovary syndrome (PCOS) and metabolic syndrome. A pivotal study led by researchers Wu and Mao dives deep into the associations between plasma extracellular vesicles long non-coding RNAs (lncRNAs) and metabolic syndrome within the context of PCOS. This analysis not only augments our comprehensive understanding but also brings a fresh perspective on potential therapeutic avenues. The ramifications of these findings could herald transformative approaches for millions affected by these interconnected disorders.
Polycystic ovary syndrome is a multifaceted endocrine disorder characterized by hormonal imbalances, ovulatory dysfunction, and polycystic ovaries. It is a prevalent condition impacting approximately 1 in 10 women of reproductive age. Beyond the reproductive health challenges, PCOS is closely linked to various metabolic concerns, including insulin resistance, obesity, and dyslipidemia. As a result, the urgency to shed light on the molecular underpinnings of this syndrome has never been more pressing.
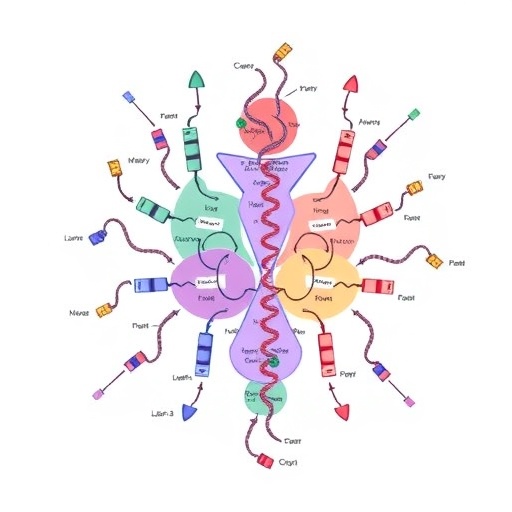
Extracellular vesicles (EVs), particularly their lncRNA content, have emerged as significant players in intercellular communication. These vesicles serve as carriers of genetic information, proteins, and lipids, facilitating the transfer of biological signals between cells. Given their expansive roles, researchers have hypothesized that the lncRNAs within EVs might act as biomarkers or even functional mediators in metabolic pathways associated with PCOS.
The study meticulously examined blood samples from PCOS patients, isolating EVs and subsequently analyzing their lncRNA profiles. The researchers discovered compelling correlations between specific lncRNAs and markers indicative of metabolic syndrome, such as insulin levels and lipid profiles. This groundbreaking link suggests that lncRNAs could serve as early indicators of metabolic complications in PCOS patients, potentially allowing for preemptive interventions.
The implications of these findings stretch far beyond mere academic interest; they open new avenues for clinical application. With the ability to detect lncRNA signatures in blood samples, healthcare providers may soon have a tool to identify at-risk patients before they manifest alarming symptoms of metabolic syndrome. Consequently, this could accelerate the implementation of lifestyle interventions or pharmacologic treatments aimed at mitigating long-term health risks.
In addition to the diagnostic potential, the study posits that lncRNAs could play a role in the pathophysiology of both PCOS and metabolic syndrome. For example, certain lncRNAs wield regulatory influences over key metabolic processes, like glucose metabolism and lipid synthesis. By understanding these functional roles, researchers could identify potential targets for novel therapeutic strategies, paving the way for personalized medicine in the domain of reproductive health.
Interestingly, the study drew attention to the biological mechanisms that underpin the association between EV lncRNAs and metabolic processes in PCOS. The researchers highlighted pathways involving inflammation and insulin signaling, which are central to both the metabolic syndrome and PCOS. This indicates that lncRNAs may not only act as passive markers but could actively contribute to the disease mechanisms, suggesting a dual role in pathology and diagnosis.
Moreover, what makes this study groundbreaking is not just its findings but also its approach. By employing cutting-edge technologies in RNA sequencing and bioinformatics, the authors succeeded in generating a comprehensive profile of lncRNAs in EVs. This adds an additional layer of credibility to their conclusions, showcasing the impressive capabilities researchers have today in elucidating complex biological systems.
Further exploration is warranted, particularly expanding the study’s population size to validate these findings across diverse demographics. Different ethnicities and age groups may reveal variable associations between lncRNAs and metabolic syndrome, enhancing our understanding of how PCOS manifests in various populations. Hence, future studies could provide a more universal framework for diagnosis and treatment.
As the research community continues to unveil these complex linkages, the hope is to translate these findings into tangible clinical practices. The emergence of personalized medicine emphasizes the necessity of individualized approaches tailored to specific patient profiles. With lncRNAs as focal points, there is optimism that specific interventions can be deployed for those exhibiting early signs of metabolic disturbance associated with PCOS.
In conclusion, Wu and Mao’s study offers a significant leap forward in our understanding of the multifactorial relationship between PCOS and metabolic syndrome. By detailing the involvement of plasma extracellular vesicles lncRNAs, the research not only provides critical insights into pathophysiological connections but also outlines a potential roadmap for diagnostic and therapeutic advancements. As the research field progresses, findings like these underscore the endless possibilities within biomedical research and their implications for women’s health on a global scale.
The intricate web binding together lncRNAs, EVs, and metabolic syndrome within the milieu of PCOS demands further investigation and rigorous exploration. The initial discoveries serve as a clarion call for researchers and clinicians alike to innovate, strategize, and collaborate in order to tackle these complex health issues head-on.
The future of how we approach PCOS is rapidly evolving. With potential biomarkers like lncRNAs emerging from studies like Wu and Mao’s, this revolution in understanding could reshuffle the existing paradigms in diagnosis and treatment. The horizon indeed looks promising for women suffering from PCOS, where early detection and tailored interventions may soon become standard practice, thus enhancing quality of life and reducing long-term health risks.
Subject of Research: The relationship between plasma extracellular vesicles lncRNAs and metabolic syndrome in polycystic ovary syndrome.
Article Title: Association between plasma extracellular vesicles LncRNAs and metabolic syndrome in polycystic ovary syndrome.
Article References:
Wu, Yz., Mao, Ll. Association between plasma extracellular vesicles LncRNAs and metabolic syndrome in polycystic ovary syndrome.
J Ovarian Res 18, 243 (2025). https://doi.org/10.1186/s13048-025-01801-4
Image Credits: AI Generated
DOI: https://doi.org/10.1186/s13048-025-01801-4
Keywords: PCOS, metabolic syndrome, extracellular vesicles, lncRNAs, biomarkers, women’s health, reproductive endocrinology.
Tags: dyslipidemia in polycystic ovary syndromeextracellular vesicles in PCOShormonal imbalances in PCOSinsulin resistance in womenintercellular communication and EVslong non-coding RNAs and metabolic syndromemolecular mechanisms of PCOSobesity and PCOS connectionPCOS prevalence among womenpolycystic ovary syndrome researchreproductive health and lncRNAstherapeutic approaches for metabolic syndrome