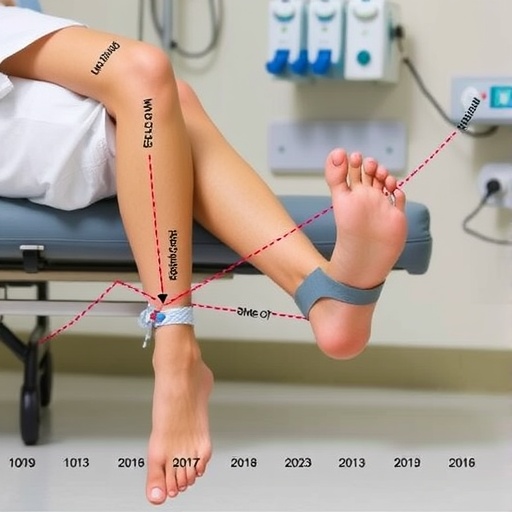
In a striking revelation from a recent comprehensive study conducted by Northwestern Medicine, the rates of leg and foot amputations have surged by a staggering 65% in Illinois hospitals between 2016 and 2023. This alarming trend underscores a growing public health crisis largely driven by the escalating prevalence of diabetes and peripheral artery disease (PAD), two chronic conditions intimately linked with lower extremity amputations. The data reveal troubling disparities, with men, Black Americans, and residents of socioeconomically disadvantaged areas disproportionately bearing the burden of these devastating outcomes.
The study, led by Dr. Maggie Reilly, a vascular surgery resident at Northwestern University’s McGaw Medical Center, delves into the complex interplay of pathophysiology, social determinants of health, and healthcare access. Vascular complications stemming from diabetes and PAD often manifest late, when patients present with severe foot wounds or ascending infections that leave limb amputation as the only viable intervention. This progression underscores the critical need for earlier diagnosis and intervention, yet the findings affirm a grim reality: many patients remain undiagnosed or inadequately managed until irreversible damage has occurred.
Despite national advances in smoking reduction and enhanced medical therapies such as statin use aimed at preserving limb function, the rapid rise in diabetes and PAD is eclipsing these gains. Statins, for example, have demonstrated efficacy in reducing cardiovascular events and improving endothelial function, but their benefits appear insufficient against the backdrop of increasing metabolic disease prevalence. Dr. Reilly emphasizes that these interventions have yet to meaningfully penetrate all communities, particularly marginalized populations, reinforcing systemic inequities that perpetuate health disparities and hinder progress in limb salvage.
The aftermath of lower limb amputation extends beyond the surgical suite. Postoperative recovery is protracted, often requiring a minimum of three months of intensive wound care and medical follow-up to promote healing. Following this, patients embark on extended regimens of physical and occupational therapy aimed at adapting to prosthetic limbs. The delay in prosthesis fitting, sometimes approaching six months, imposes significant physical debilitation, exacerbating muscle atrophy and reducing overall mobility. This rehabilitation phase demands a multidisciplinary approach involving surgeons, therapists, and social supports to restore independent functioning and quality of life.
Psychological ramifications compound the physical challenges faced by amputees. Patients frequently endure profound mental distress, grappling with feelings of shame, loss, and disenfranchisement with the healthcare system. The progressive and chronic nature of diabetes and PAD often confounds patients’ understanding of their disease trajectory, complicating acceptance and adaptation to limb loss. This psychosocial burden highlights the necessity for integrated mental health services alongside medical care to address the holistic needs of this vulnerable population.
Although Illinois served as the focus of this inquiry, the study’s authors contend that these rising amputation rates likely mirror national trends, given the state’s demographic heterogeneity encompassing urban, suburban, and rural communities as well as diverse racial and ethnic groups. The data stem from 30,834 amputation admissions across 193 hospitals, revealing a 65% increase in annual amputation rates over the observed period. Notably, amputees were predominantly male (71.2%) and disproportionately represented non-Hispanic Black patients, who accounted for 25% of amputations despite comprising only 13.9% of Illinois residents in the 2020 census.
The mortality associated with above-knee amputations is sobering, with approximately half of patients succumbing within 12 months post-operation due to systemic complications and comorbidities. This statistic underscores the exigency of preventative strategies targeting early detection and aggressive management of cardiovascular risk factors, particularly in underserved populations where PAD remains frequently underrecognized and undertreated. Screening programs, community outreach, and tailored interventions are critical components in curbing this trajectory.
Key findings from the study reveal nuanced demographic and clinical trends. The largest surges in amputation rates occurred among males, with an increase of 76.1%, and non-Hispanic Black patients, who experienced a 67.5% rise. Age groups most affected included individuals between 65 and 74 years old, highlighting an urgent need to focus on older adults who bear compounded risks from aging vasculature and metabolic disorders. Additionally, hospital stays extending beyond 20 days escalated, reflecting the complexity and severity of presentations.
The pathophysiological nexus of diabetes and PAD drives a vicious cycle of ischemia, neuropathy, and infection. Diabetes-induced microvascular damage impairs perfusion, while PAD further constricts arterial flow, collectively predisposing to trophic ulcers and gangrene. These wounds, resistant to healing due to compromised blood supply and immune dysfunction, frequently necessitate limb removal to prevent systemic sepsis. The interplay of metabolic dysregulation and atherosclerotic occlusion mandates a multifaceted approach encompassing glycemic control, lipid management, and revascularization procedures when feasible.
Addressing the stark disparities illuminated by this research requires systemic policy reforms and innovative healthcare delivery models focused on equity. Enhancing access to preventative services, expanding patient education on disease self-management, and integrating culturally competent care are pivotal. The research team highlights collaboration between health systems and community organizations as a promising avenue to dismantle barriers and ensure comprehensive risk factor management.
This population health analysis, titled “A population health analysis of trends in lower extremity amputation secondary to diabetes and peripheral artery disease, 2016–2023,” is a clarion call to confront an urgent and expanding public health crisis. Published on October 30, 2025, in the journal Diabetes Research and Clinical Practice, the study harnesses extensive hospital data to deliver nuanced insights into demographic disparities, clinical outcomes, and opportunities for intervention.
Ultimately, this study portrays a health crisis at the intersection of chronic disease, social inequity, and healthcare system limitations. The accelerating rates of amputations stand as a stark barometer of systemic failures in chronic disease management and preventive care. To reverse this trend, multidisciplinary efforts emphasizing early screening, community engagement, individualized risk reduction, and equitable resource distribution are imperative. Without targeted action, the divide in amputation rates among marginalized populations will widen, tragically perpetuating preventable disability and mortality on a national scale.
Subject of Research: People
Article Title: A population health analysis of trends in lower extremity amputation secondary to diabetes and peripheral artery disease, 2016–2023
News Publication Date: 30-Oct-2025
Web References: Diabetes Research and Clinical Practice – DOI: 10.1016/j.diabres.2025.112963
Keywords: Amputation, Surgical procedures, Diabetes, Peripheral nervous system, Cardiology, Cardiovascular disorders
Tags: chronic conditions leading to amputationsearly diagnosis and intervention in PADfoot amputation statistics 2023health disparities in amputation rateshealthcare access and outcomesimpact of diabetes on limb healthleg amputation rates in Illinoisperipheral artery disease and amputationspublic health crisis in diabetesracial disparities in healthcare outcomessocial determinants of health in Illinoisvascular surgery trends in hospitals