In a groundbreaking discovery that promises to reshape current understanding of autoimmune kidney diseases, a team of researchers has unveiled a novel metabolic communication pathway linking mesangial cells to the immune system’s adaptive arm in lupus nephritis. The study, recently published in Nature Communications, reveals how lactate functions not merely as a metabolic byproduct but as a critical signaling molecule that orchestrates the differentiation of follicular helper T cells (Tfh), a specialized subset of immune cells implicated in autoantibody production and disease progression in lupus nephritis.
Lupus nephritis, a serious manifestation of systemic lupus erythematosus (SLE), involves immune-mediated damage of the kidney’s glomerular filtration system, particularly affecting mesangial cells. These specialized cells, situated within the glomerulus, play essential roles in maintaining structural integrity and modulating local immune responses. Traditional views have largely considered mesangial cells as passive victims of immune attack, but mounting evidence suggests they actively participate in the disease microenvironment through complex signaling networks.
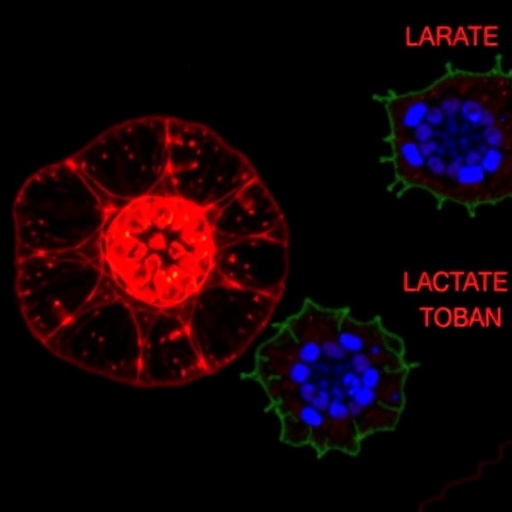
The newly reported findings pivot around lactate, a metabolite long regarded as a waste product of anaerobic glycolysis. The research team led by Liu, Ji, and Lei challenges this outdated paradigm by demonstrating that lactate released by activated mesangial cells acts as a molecular bridge facilitating crosstalk with the immune system’s T helper cells. This intercellular communication primes a subset of naïve CD4+ T cells to differentiate into Tfh cells within the renal microenvironment, thereby exacerbating autoimmune inflammation locally.
Employing cutting-edge single-cell RNA sequencing and metabolic flux analysis, the study maps an intricate lactate-mediated signaling cascade. Mesangial cells undergoing metabolic reprogramming in lupus nephritis secrete elevated lactate levels, which are sensed by nearby T cells through specific lactate transporters and G-protein coupled receptor pathways. This interaction notably enhances the expression of BCL6, the transcription factor considered the master regulator of Tfh cell differentiation, as well as the secretion of interleukin-21, a cytokine critical for B cell help and autoantibody maturation.
The temporal and spatial precision of this lactate-mediated dialog emerged from sophisticated in vivo imaging and organoid culture systems, which mimic the unique architecture of renal glomeruli. These models confirmed that localized lactate accumulation creates a permissive niche fostering Tfh cell expansion and sustained autoimmune activation. Significantly, the research underscores the pathological importance of metabolic microenvironment remodeling in lupus nephritis, emphasizing lactate not simply as a passive player but as a pivotal immunometabolic modulator.
These insights open exciting prospects for novel therapeutic approaches aimed at disrupting this pathological metabolic-immune axis. Targeting lactate production or blocking its sensing mechanisms in immune cells could offer a new class of interventions designed to attenuate Tfh-mediated autoimmunity, thereby reducing kidney damage and improving clinical outcomes. Unlike conventional immunosuppressive therapies, which broadly dampen immune responses, metabolic intervention offers a potentially more selective strategy with fewer side effects.
Moreover, the discovery sheds light on the broader relevance of metabolic regulation in autoimmunity beyond the renal microenvironment. The emerging concept that tissue-resident non-immune cells actively shape immune landscapes through metabolic cues may have implications across diverse autoimmune disorders and inflammatory pathologies. This lactate-centric paradigm invites a reexamination of disease mechanisms and encourages exploration of metabolic checkpoints as new therapeutic targets.
The methodology employed in the study demonstrated remarkable innovation, combining transcriptomic, proteomic, and metabolic profiling with functional immunology assays in patient-derived samples and murine lupus models. This integrative approach allowed the researchers to dissect cell-type-specific contributions and the dynamic interplay between metabolism and immune cell differentiation in unprecedented detail, setting a new standard for immunometabolic research.
Significantly, the study’s findings emphasize the bidirectional nature of immune and metabolic communication in the kidney. While immune cells influence mesangial cell phenotypes, mesangial cells reciprocate through metabolic signals, effectively creating a feedback loop that sustains chronic inflammation. Understanding this reciprocal dialogue is crucial for envisioning strategies to break the cycle of injury and repair in lupus nephritis.
Furthermore, the work revisits the role of lactate beyond its traditional view as a byproduct of hypoxia or inflammation. It emerges here as a bona fide immunotransmitter that modulates fate decisions within the T cell compartment, reinforcing a growing recognition that metabolic intermediates serve as signaling molecules with profound effects on immune cell behavior. This positions lactate alongside other metabolites such as succinate and fumarate, which are key regulators in immunometabolism.
Lactate’s role in promoting Tfh differentiation aligns with burgeoning data implicating metabolic states in guiding T cell lineage specification. By elucidating a kidney-specific pathway, the research brings into focus how local tissue metabolism sculpts immune responses uniquely tailored to the renal environment, which is characterized by its distinctive oxygen tension, nutrient availability, and cellular composition.
The clinical implications of this study are immense. Since Tfh cells play a pivotal role in autoantibody production—a hallmark of lupus nephritis—the identification of metabolic inputs regulating their differentiation highlights new biomarkers and intervention points. Non-invasive monitoring of lactate levels or lactate signaling components might serve as disease activity indicators or therapeutic response predictors in lupus nephritis patients.
Looking forward, the findings prompt important questions about how systemic metabolic derangements common in lupus patients, such as altered glucose metabolism and mitochondrial dysfunction, integrate with local tissue signals to modulate immune responses. Understanding the intersection of systemic and tissue-specific metabolism in lupus could drive holistic approaches targeting both systemic and organ-specific pathogenic mechanisms.
Importantly, this research reiterates the necessity of viewing autoimmune diseases through a multifaceted lens encompassing immunology, metabolism, and tissue biology. The crosstalk between mesangial cells and immune effectors mediated by lactate exemplifies the complexity of autoimmunity and introduces a paradigm where non-immune metabolic actors critically dictate immune function and disease progression.
As further studies expand on these findings, the potential to harness metabolic reprogramming both to mitigate immune dysregulation and promote tissue homeostasis represents a promising frontier. This could herald an era of precision medicine where metabolic modulation complements immunotherapy to achieve durable remission in lupus nephritis and related autoimmune disorders.
In conclusion, the revelation that lactate serves as a conduit linking mesangial cells to Tfh cell differentiation not only deepens the mechanistic understanding of lupus nephritis but also underscores metabolism as a fertile ground for innovative therapeutic strategies. This landmark study by Liu, Ji, Lei, and colleagues marks a significant advance, highlighting how metabolic pathways rewire immune circuits to drive chronic kidney inflammation and autoimmunity with potential implications far beyond lupus nephritis.
Subject of Research:
The metabolic and immunological interaction between mesangial cells and follicular helper T cells in the pathogenesis of lupus nephritis.
Article Title:
Lactate bridges mesangial cells to the differentiation of follicular helper T cells in lupus nephritis.
Article References:
Liu, M., Ji, H., Lei, J. et al. Lactate bridges mesangial cells to the differentiation of follicular helper T cells in lupus nephritis. Nat Commun (2025). https://doi.org/10.1038/s41467-025-67416-x
Image Credits: AI Generated
Tags: autoimmune kidney disease researchfollicular helper T cells role in lupusimmune-mediated kidney damageimplications of mesangial cell activitykidney glomerulus immune responselactate as a signaling moleculelactate signaling in autoimmune diseasesmesangial cells and immune interactionmetabolic communication in kidney diseasenovel therapeutic targets in lupussystemic lupus erythematosus pathophysiologyT cell differentiation in lupus nephritis