Patients with congestive heart failure (CHF) having a compromised blood supply, are at greater risk of sudden cardiac death (SCD). With an estimated incidence as high as 22% among these patients, current clinical guidelines recommend using implantable cardioverter defibrillators (ICDs) to help mitigate the risk of SCD.
Credit: Yoshihiro Sobue from Fujita Health University
Patients with congestive heart failure (CHF) having a compromised blood supply, are at greater risk of sudden cardiac death (SCD). With an estimated incidence as high as 22% among these patients, current clinical guidelines recommend using implantable cardioverter defibrillators (ICDs) to help mitigate the risk of SCD.
Although the application of ICDs in patients with CHF is backed by substantial evidence, these studies did not include people with chronic kidney disease (CKD), who are an important clinical population. In other words, it is unclear whether the use of ICDs is justified in patients with CKD, especially with mild and moderate presentations, given the inherent risk involved in installing these devices.
To address this knowledge gap, researchers led by Associate Professor Yoshihiro Sobue from Fujita Health University, Japan, investigated to what extent kidney function can be a good predictor for the risk of SCD. This study was published in ESC Heart Failure on June 10 2024, and was co-authored by Hideo Izawa, also from Fujita Health University, and Eiichi Watanabe from Fujita Health University Bantane Hospital.
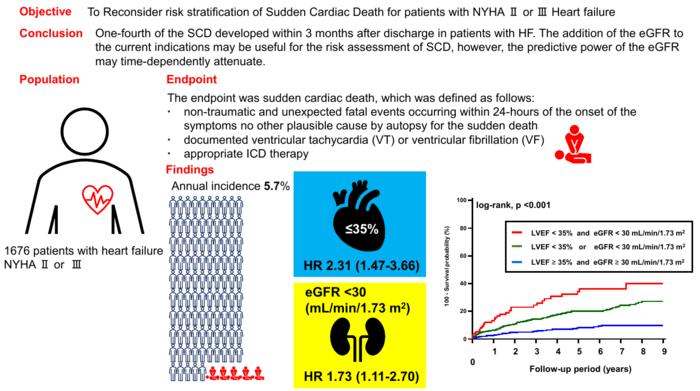
Elaborating on the rationale behind this examination, Dr. Sobue says, “The objective of our study was to prospectively investigate the risk factors for SCD in a cohort of over 1,500 patients hospitalized with CHF classified based on the left ventricular ejection fraction (LVEF) and the New York Heart Association (NYHA) functional class, as well as the potential role of kidney function as a determinant of SCD.” Adding further on the importance of using renal dysfunction for SCD, he says, “The determination of renal dysfunction as an independent risk factor of SCD is important because patients with moderate-to-severe renal dysfunction were excluded in the studies on which current ICD implantation guidelines are based.”
The study ultimately included 1,676 patients who had visited Fujita Health University Hospital for decompensated heart failure. During the follow-up period, 198 of these patients suffered from SCD. Among these events, 23% occurred within 3 months of discharge.
On conducting statistical analyses of the gathered data, the research team identified two key independent predictors for the risk of SCD following discharge. The first was LVEF, which is already considered in the current guidelines. The second was the estimated glomerular filtration rate (eGFR), which is a measure of how well the kidneys can filter blood.
By adding eGFR as a predictor alongside LVEF, regression models could predict SCD more accurately. However, as the researchers noted, the predictive power of kidney function in this way diminished over time, being more effective in the first few months after discharge. Coincidentally, roughly a quarter of all cases of SCD occurred within three months of discharge.
In summary, the findings of this study underline the importance of considering additional factors, such as kidney condition, when weighing the benefits of using ICD in a patient. “Refining the criteria for ICD implantation holds the potential for significantly improving the prevention of SCD and reducing the incidence of complications arising from unnecessary ICD implantations. Hopefully, applying an enhanced stratification methodology involving eGFR may yield better clinical outcomes,” remarks Dr. Sobue.
In the long term, these findings may steer the way for the revision of guidelines for the use of ICDs and improve the outcomes for patients with CHF, both with and without CKD.
***
Reference
Title of original paper: Renal dysfunction is a time-varying risk predictor of sudden cardiac death in heart failure
Journal: ESC Heart Failure
DOI: https://doi.org/10.1002/ehf2.14892
About Fujita Health University
Fujita Health University is a private university situated in Toyoake, Aichi, Japan. It was founded in 1964 and houses one of the largest teaching university hospitals in Japan in terms of the number of beds. With over 900 faculty members, the university is committed to providing various academic opportunities to students internationally. Fujita Health University has been ranked eighth among all universities and second among all private universities in Japan in the 2020 Times Higher Education (THE) World University Rankings. THE University Impact Rankings 2019 visualized university initiatives for sustainable development goals (SDGs). For the “good health and well-being” SDG, Fujita Health University was ranked second among all universities and number one among private universities in Japan. The university became the first Japanese university to host the “THE Asia Universities Summit” in June 2021. The university’s founding philosophy is “Our creativity for the people (DOKUSOU-ICHIRI),” which reflects the belief that, as with the university’s alumni and alumnae, current students also unlock their future by leveraging their creativity.
Website: https://www.fujita-hu.ac.jp/en/index.html
About Associate Professor Yoshihiro Sobue from Fujita Health University
Dr. Yoshihiro Sobue currently serves as an Associate Professor at the Department of Cardiology of Fujita Health University. He specializes in cardiac pathophysiology and epidemiology, as well as other aspects of cardiology. He has published over 40 research papers on these topics.
Funding information
Dr. Izawa—one of the authors—received grant support through his institution from Bayer, Daiichi-Sankyo, Sumitomo Dainippon, Kowa, Ono, Otsuka, Takeda and Fujifilm Toyama Kagaku and honoraria for lectures from Otsuka, Novartis, Eli Lilly Japan, Bayer and Daiichi-Sankyo.
Journal
ESC Heart Failure
DOI
10.1002/ehf2.14892
Method of Research
Observational study
Subject of Research
People
Article Title
Renal dysfunction is a time-varying risk predictor of sudden cardiac death in heart failure
Article Publication Date
10-Jun-2024
COI Statement
Dr. Watanabe is a recipient of lecture fees from Daiichi-Sankyo and research funding from Boehringer Ingelheim, Takeda Pharmaceutical Company, Japan Lifeline, Medtronic Japan, Boston Scientific Japan, Biotronik Japan and St. Jude Medical Japan. Dr. Izawa has received grant support through his institution from Bayer, Daiichi-Sankyo, Sumitomo Dainippon, Kowa, Ono, Otsuka, Takeda and Fujifilm Toyama Kagaku and honoraria for lectures from Otsuka, Novartis, Eli Lilly Japan, Bayer, and Daiichi-Sankyo.




