The human gut microbiome, a complex ecosystem of trillions of microorganisms, plays a crucial role in maintaining various bodily functions, particularly in digestion and immune response. Among these, the bacterium Clostridium scindens has caught the attention of researchers exploring its potential therapeutic effects on inflammatory conditions such as ulcerative colitis (UC). This chronic disease leads to inflammation of the colon, resulting in significant discomfort and a lower quality of life for affected individuals. Current treatment options often involve immune suppression and provide limited relief, underscoring the urgent need for novel approaches aimed at restoring gut health.
Recent findings from the laboratories of Kristina Schoonjans and Rizlan Bernier-Latmani at the École Polytechnique Fédérale de Lausanne (EPFL) shed light on the biochemical roles of specific gut bacteria, particularly focusing on bile acids, which are critical for fat digestion and overall intestinal health. Patients suffering from UC typically exhibit low levels of microbiome-derived bile acids, which raises questions about whether restoring these compounds could facilitate healing in the intestinal lining. Bile acids serve not only as digestive agents but also as signaling molecules that help regulate various intestinal functions.
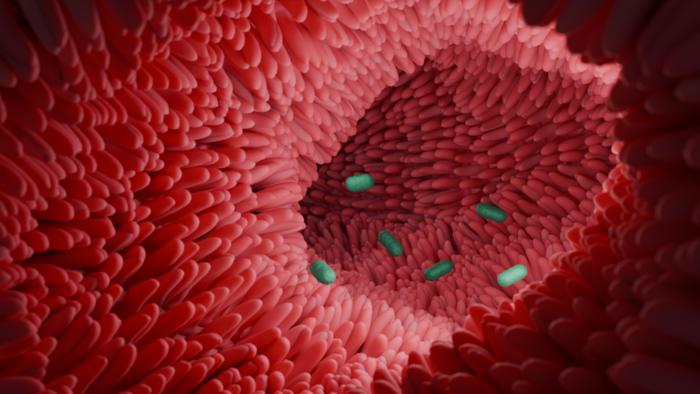
In their groundbreaking study, the researchers discovered that Clostridium scindens functions as a bile acid converter, transforming primary bile acids into 7α-dehydroxylated bile acids, which are linked to improved mucosal healing in the intestine. By examining an animal model of colitis that closely mimics the manifestations of UC, the team introduced this beneficial bacterium into a select group of mice while leaving others untreated. The results were telling; those mice that received Clostridium scindens exhibited accelerated recovery, with significantly reduced inflammation and improved regeneration of the gut lining.
A critical component of this recovery process was identified as TGR5, a receptor that responds to the varied forms of bile acids, including those produced by Clostridium scindens. This receptor plays a significant role in stimulating the proliferation and differentiation of intestinal stem cells. Further investigations confirmed that when mice deficient in TGR5 were treated with Clostridium scindens, the positive effects on gut health were markedly diminished. Through this pathway, the research established a crucial link between bile acid metabolism and the gut’s inherent healing capabilities.
Translating these findings to human applications, researchers analyzed patient data to assess the relevance of their animal studies. They found a compelling correlation between lower levels of 7α-dehydroxylated bile acids and impaired intestinal cell renewal among UC patients. This discovery highlights the potential promise of using microbiome-targeted strategies to restore bile acid metabolism and enhance intestinal healing. As pointed out by Antoine Jalil, one of the study’s authors, these results reveal a pivotal avenue for diverting from conventional therapies that primarily aim to suppress inflammation.
Moreover, backtracking and examining how gut microbiota contributes to overall gut health, the roles played by various bacterial species—in this case, Clostridium scindens—become essential. Gut dysbiosis, an imbalance of the microbiome, occurs in many patients with inflammatory bowel disease, creating a twofold problem of impaired healing and increased susceptibility to further inflammation. The new insights into how specific bacteria can modify bile acids open an exciting frontier in microbiome research, with implications beyond UC alone.
In conclusion, this research does not just illuminate the interactions between microbes and their human hosts. It opens pathways towards integrating microbiome-focused therapies that harness the body’s natural mechanisms to recover from disease. As scientists pinpoint the roles of these microbial agents, future investigations could lay the groundwork for a revolution in understanding gastrointestinal disorders. The healing potential of beneficial bacteria like Clostridium scindens is just the beginning, and this represents a significant leap toward personalized medicine in treating chronic inflammatory conditions.
The broader implications of these findings resonate beyond ulcerative colitis, pointing toward new methodologies applicable to a multitude of gastrointestinal disorders. This burgeoning field of microbiome research may redefine how we understand the intricate relationship between our health and the microorganisms inhabiting our bodies. As scientists continue untangling this complex web of interaction, the prospect of microbiome-targeted therapies appears not only feasible but potentially transformative in the realm of medicine.
Subject of Research: The role of Clostridium scindens in bile acid metabolism and gut healing in ulcerative colitis.
Article Title: Bile acid 7α-dehydroxylating bacteria accelerate injury-induced mucosal healing in the colon.
News Publication Date: March 10, 2025.
Web References: 10.1038/s44321-025-00202-w
References: Antoine Jalil, Alessia Perino, Yuan Dong, Jéromine Imbach, Colin Volet, Eduard Vico-Oton, Hadrien Demagny, Lucie Plantade, Hector Gallart-Ayala, Julijana Ivanisevic, Rizlan Bernier-Latmani, Siegfried Hapfelmeier, Kristina Schoonjans. (2025). Bile acid 7α-dehydroxylating bacteria accelerate injury-induced mucosal healing in the colon. EMBO Molecular Medicine.
Image Credits: Credit: K. Schoonjans (EPFL).
Keywords: Clostridium scindens, ulcerative colitis, bile acids, gut microbiome, intestinal healing, TGR5, inflammation, microbiome-targeted therapy, mucosal healing.
Tags: bile acids and digestionchronic colon inflammationClostridium scindens therapeutic effectsgut bacteria and signaling moleculesgut health and diseaseimmune response and microbiotainflammatory bowel disease researchintestinal microbiotamicrobiome-derived compoundsnovel treatment approaches for UCrestoring gut healthulcerative colitis management