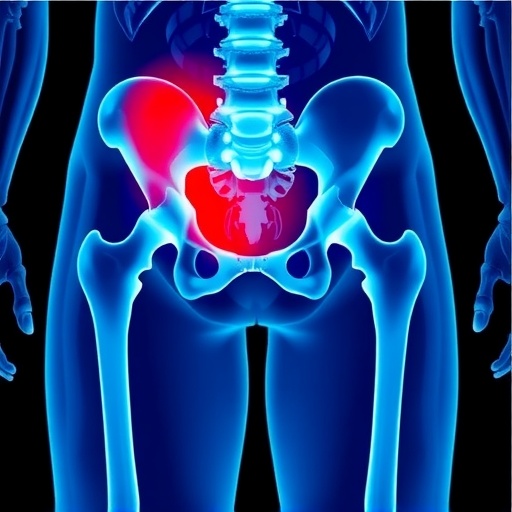
In a groundbreaking study published in Archives of Osteoporosis, researchers led by Dr. Jing Cheng unveiled an innovative integrated ortho-internal model that has the potential to significantly reduce mortality rates in elderly patients suffering from high-risk hip fractures. This research addresses a critical public health issue, as hip fractures in the aged population not only lead to high rates of morbidity but also carry a looming risk of mortality that demands immediate attention from both medical professionals and caregivers.
Hip fractures are notorious for their devastating effects on the elderly, often leading to prolonged hospital stays, loss of independence, and, tragically, increased mortality. Current treatment paradigms may not adequately address the complex interplay of medical, surgical, and rehabilitative care needed for optimal recovery in these vulnerable patients. The integrated ortho-internal model proposed by Cheng and colleagues aims to streamline and enhance these processes, emphasizing a holistic approach to treatment.
At the core of this scientific endeavor is a robust framework that combines orthopedic surgery, internal medicine, and physiotherapy. This integrative model not only focuses on the immediate surgical intervention following a hip fracture but also incorporates pre-operative risk assessments and post-operative rehabilitation strategies. This multifaceted approach acknowledges that the management of hip fractures in older individuals cannot be one-dimensional; instead, it requires a coordinated effort from various healthcare disciplines to improve patient outcomes.
The researchers conducted a comprehensive analysis involving a cohort of high-risk elderly patients, all of whom experienced hip fractures. They meticulously tracked various parameters, including mortality rates, recovery times, and overall quality of life post-surgery. What emerged from the data was promising: those treated within the integrated ortho-internal framework demonstrated significantly reduced mortality rates compared to those who received standard care.
A key component of the model is the incorporation of predictive analytics into the pre-operative evaluation of patients. By utilizing advanced algorithms that analyze patient data—such as comorbidities, functional status, and even socio-economic factors—physicians can identify patients with the highest risk profiles for adverse outcomes. This enables targeted interventions that are tailored to individual needs, ultimately improving outcomes and enhancing recovery processes.
The post-operative phase of care within this integrated model was equally impressive. Patients received customized rehabilitation plans that accounted for their unique medical histories and injury profiles. This included specialized physical therapy regimens designed to bolster strength and mobility while minimizing the chances of complications such as pneumonia or deep vein thrombosis, which are prevalent risks for hospitalized elderly patients.
Additionally, Cheng and her team underscored the importance of psychological support during recovery. The integrated model incorporates mental health evaluations to address potential issues of depression and anxiety that are often overlooked in the context of physical rehabilitation. This holistic view ensures that patients are not just physically rehabilitated but also supported emotionally, leading to a better overall recovery experience.
In a society that is rapidly aging, addressing the challenges posed by hip fractures is more crucial than ever. This integrated ortho-internal model could be pivotal in transforming the way healthcare systems approach elderly care. It suggests a paradigm shift from reactive, surgical interventions to a more proactive, comprehensive strategy that keeps the patient’s entire well-being in focus.
The implications of this research extend beyond individual patient care. If implemented widely, the integrated ortho-internal model could reduce the healthcare burden associated with hip fractures, potentially saving millions of healthcare dollars traditionally spent on extended hospital stays, rehabilitation, and follow-up care due to complications. The economic benefits, coupled with improved patient outcomes, make a compelling case for healthcare systems to consider such integrative frameworks.
Overall, the study conducted by Cheng, Chao, Ren, and their colleagues is not just an academic exercise; it heralds a new era of clinical practice in the treatment of elderly patients with hip fractures. As the population ages and the incidence of such injuries continues to rise, healthcare providers are challenged to innovate and adapt. This research is a beacon of hope, offering a blueprint for a more effective, patient-centered approach to a deeply entrenched medical challenge.
In conclusion, the integrated ortho-internal model represents a forward-thinking strategy that could fundamentally alter the landscape of elderly hip fracture management. This dual focus on surgical excellence and comprehensive post-operative care underscores an essential truth in medicine: optimal care can only be achieved through collaboration among various specialties, with the patient at the center of all decisions. As more institutions adopt this model, we may finally see a significant decline in the mortality rates associated with one of the most critical health issues facing our aging population today.
The findings from this study not only provide a roadmap for improved clinical practices but also invite further investigations into how similar integrative models can be applied to other high-risk conditions affecting the elderly. As healthcare professionals continue to grapple with the complexities of geriatric care, the call for innovative solutions like the integrated ortho-internal model will resonate ever louder.
Subject of Research: Integrated ortho-internal model for reducing mortality in high-risk aged hip fractures.
Article Title: Integrated ortho-internal model reduces mortality in high-risk aged hip fractures.
Article References:
Cheng, J., Chao, AJ., Ren, Z. et al. Integrated ortho-internal model reduces mortality in high-risk aged hip fractures.
Arch Osteoporos 21, 17 (2026). https://doi.org/10.1007/s11657-025-01641-1
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s11657-025-01641-1
Keywords: Hip Fractures, Elderly Care, Integrated Healthcare Model, Orthopedics, Rehabilitation, Mortality Reduction.